 |
 |
| jbm > Volume 31(1); 2024 > Article |
|
Abstract
Background
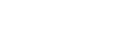
In this pre-planned variation of the Comparing Strategies Targeting Osteoporosis to Prevent Fractures After an Upper Extremity Fracture (C-STOP) trial, we investigated whether adherence-specific coaching by the case manager (CM) further improved the adherence and persistence rates compared to those seen in the C-STOP trial.
Methods
We conducted a prospective observational cohort study of community-dwelling adults 50 years or older who suffered an upper-extremity fracture and were not previously treated with osteoporosis medications, to assess whether a well-trained CM can partner with patients to improve adherence to and persistence with oral bisphosphonate intake. The primary outcome was adherence (taking > 80% of prescribed doses) to oral bisphosphonate intake at 12 months after study enrollment. Secondary outcomes included primary adherence to and 12-month persistence with oral bisphosphonate and calcium and vitamin D supplement intake at 12 months.
Results
The study cohort consisted of 84 participants, of which 30 were prescribed an oral bisphosphonate. Twenty-two (73.3%) started treatment within 3 months. The adherence rate at 12 months was 77.3%. The persistence rate at 12 months was 95.5%. Of those not prescribed an oral bisphosphonate, 62.8% were taking supplemental calcium and 93.0% were taking supplemental vitamin D at 12 months. Depression was a significant predictor of 12-month non-adherence (adjusted odds ratio, 9.8; 95% confidence interval, 1.2-81.5).
Osteoporosis is a clinically silent disease until it leads to a fracture. Worldwide, one in three women and one in five men will suffer a fracture after the age of 50 years, 80% of those who have suffered a fracture are neither identified nor treated for osteoporosis pre-fracture.[1] Patients with an index fracture, particularly those of the upper extremity, are more likely to sustain subsequent more serious fractures at the hip or vertebrae which are associated with significant morbidity and mortality.[2-4]
Despite having medications, such as bisphosphonates, that are efficacious at preventing bone loss and fractures, suboptimal treatment rates are further attenuated by poor medication adherence and persistence.[5,6] In our original Comparing Strategies Targeting Osteoporosis to Prevent Fractures After an Upper Extremity Fracture (C-STOP) trial, we found that a nurse case manager (CM) could significantly increase testing for osteoporosis by 17% and starting treatment by 70% compared with an enhanced usual care control group.[7] Twelve-month adherence rates were high (79%) in both the active control group and the CM group in the C-STOP trial.
In this study, we evaluate if a well-trained CM with a specific focus on promoting adherence and persistence to osteoporosis medications through close follow-up and adherence-specific counseling can further improve adherence and persistence rates compared to those seen in the C-STOP trial.
Edmonton is the fifth largest city in Canada and has a metropolitan population of approximately 1.4 million in 2021.[8] All residents have access to publicly funded healthcare and all individuals over the age of 65 years have their medication costs covered by government subsidy through Alberta Blue Cross. Individuals under the age of 65 years either pay out-of-pocket or have private insurance for medication costs.
Community-dwelling adults 50 years or older who suffered an upper extremity fracture (distal radius and/or ulna, or proximal humerus fracture) not due to major trauma or pathologic fracture and presented to the Emergency Department or Fracture Cast Clinic of a tertiary care university hospital in Edmonton, Canada were recruited between 22 January 2018 and 27 February 2019. Patients were excluded if they met any of the following criteria: currently receiving osteoporosis therapy, previously documented allergy to bisphosphonates, resident of a nursing home or long-term care facility, reside outside the Greater Edmonton Area, currently enrolled in another osteoporosis study, unable to read or converse in English, unable or unwilling to participate.
We conducted a prospective observational cohort study to test whether a CM can partner with patients to improve adherence and persistence to oral bisphosphonate by using person-centered approaches. The primary outcome was adherence to oral bisphosphonate at 12 months after study enrollment. Secondary outcomes included primary adherence to oral bisphosphonate and calcium and vitamin D use at 12 months. The current study received ethics approval from the University of Alberta (PRO00018520) and was registered at ClinicalTrials.gov (NCT01401556).
The CM role was similar to that in our parent C-STOP study, which has been previously reported in detail.[7,9] Briefly, she contacted participants to arrange in clinic-visits where she educated and counseled them about osteoporosis and preventative strategies. She then arranged and interpreted bone mineral density (BMD) and laboratory tests. If participants had undergone BMD testing within 2 years before sustaining their fracture, the previous result was used for fracture risk assessment. Fracture risk assessment was completed using clinical characteristics and BMD results. Treatment was initiated for participants if their fracture risk assessment tool or Canadian Association of Radiologists and Osteoporosis Canada tool 10-year probability of major osteoporotic fracture or was greater than 20% per Canadian guidelines.[10] She counseled those who were eligible for bisphosphonate treatment about potential benefits and side effects, and provided prescriptions. She counseled all participants on adequate calcium and vitamin D intake. Referrals to an osteoporosis specialist was facilitated for those not suitable for bisphosphonate therapy or who requested a consult.
In this study, we expanded upon the CM role through more frequent telephone follow-ups (3, 6 months, and 1 year). Specific assessment and coaching around osteoporosis medication adherence and persistence took place at each planned follow-up. Any questions, details, education, or advice requested by each patient were provided at their request during each telephone call or at any time they wished to contact the CM.
Oral bisphosphonate adherence and persistence were confirmed with self-reported data and pharmacy-fill records. Calcium and vitamin D supplementation were assessed by self-report as a binary variable (taking vs. not taking) at 12 months.
Per literature-based definition,[11,12] adherence was considered positive if a patient took 80% or more of what had been prescribed. Primary adherence was considered positive if an individual started a new osteoporosis medication within 3 months of seeing the CM. Persistence was considered positive if a patient filled their osteoporosis medication within 3 months of the first prescription and was still taking the same osteoporosis medication at 1-year follow-up. Of note, a patient can be non-adherent but persistent at 12 months and vice versa.
Baseline demographics, smoking status, alcohol intake and comorbidities were reported by participants and confirmed with electronic chart review. BMD results from dual energy X-ray absorptiometry scans were obtained by electronic chart review.
Baseline characteristics were reported by 12-month bisphosphonate adherence status and 12-month calcium and vitamin D use. Continuous variables were reported as means and standard deviations. Continuous variables were compared using Student’s t-test or Wilcoxon signed-rank test, as appropriate. Categorical variables were reported as percentages and compared between groups using χ2 statistics. Logistic regression models were performed to assess predictors of adherence. Multivariable regression modeling was limited due to low cell numbers and potentially overfitting our models. The final adjusted model included age and depression. The data were analyzed using the SAS software, version 9.4 (SAS institute, Cary, NC, USA).
A total of 390 individuals were assessed for eligibility with 84 enrolled in the study. All individuals were recommended to take calcium and vitamin D supplementation per Canadian guidelines.[10] Thirty-one (36.9%) met the criteria for offering osteoporosis pharmacologic treatment, along with calcium and vitamin D supplementation. One individual was prescribed denosumab 60 mg sc every 6 months. The remaining 30 individuals were prescribed an oral bisphosphonate by the CM (Fig. 1).
Twenty-two (73.3%) of those prescribed an oral bisphosphonate (alendronate 70 mg po weekly or risedronate 35 mg po weekly) had started treatment by 3 months (primary adherence). All 22 individuals completed follow-up at 12 months. Seventeen individuals (77.3%) met the 80% definition for adherence and 21 (95.5%) were persistent with oral bisphosphonates at 12 months (Fig. 1). The only significant difference in baseline characteristics between those who were adherent and those who were non-adherent at 12 months was the presence of baseline depression (17.7% of adherence, 80.0% of non-adherent, P<0.05) (Table 1).
Of the 53 individuals not meeting criteria for pharmacologic treatment, 10 were lost to follow-up at 12-month. Of the 43 individuals who completed their 12-month follow-up, 27 (62.8%) were taking calcium supplements and 40 (93.0%) were taking vitamin D supplements at 12-month.
The only significant predictor of 12-month non-adherence was a self-reported diagnosis of depression (unadjusted odds ratio [OR], 11.7; 95% confidence interval [CI], 1.5-91.5). Depression remained a significant predictor of 12-month non-adherence after adjusting for age (adjusted OR, 9.8; 95% CI, 1.2-81.5). We were unable to adjust for sex because all non-adherent individuals were female. Other baseline characteristics were not significantly different between those who were adherent vs. non-adherent (all P>0.05).
In this study, adherence-specific coaching by an experienced nurse CM resulted in high rates of primary adherence (73%), and 12-month persistence (96%) and adherence (77%). However, these results were similar to those reported in the original C-STOP study, in which primary adherence was 78% and 12-month adherence was 79% in the CM arm.[9] Specific adherence questions and coaching by the CM did not further increase adherence to oral bisphosphonates in this population.
In the original C-STOP study, 12-month and 24-month adherence to oral bisphosphonates were similar between the CM group and the active control group.[9] The active control group consisted of the research nurse calling the participant at 2 to 4 weeks post-fracture to discuss osteoporosis and encouraging the participant to follow-up with his or her family physician. Their family physician also received a faxed patient-specific letter informing them that their patient had a fracture and included evidence-based guidelines endorsed by local opinion leaders.[13] Given both the original CM intervention and the adherence-specific CM intervention in this study were unable to further improve medication adherence, there may be an adherence ceiling through which even resource-intensive interventions cannot break.
While we were not able to further bridge the adherence gap, the 12-month-persistence rate in our cohort was very high (96%). Patients who start an osteoporosis medication continue to self-assess whether to keep taking their medication.[14] This ongoing patient self-assessment potentially provides a unique opportunity for the CM to facilitate specific clear person-centered communication techniques that confirm and reinforce patient understanding to achieve better persistence but not adherence. Exploration of the causes of non-adherence and non-persistence was outside the scope of this study. However, a previous qualitative study of 12 patients at our center found that reasons for non-compliance included perceiving osteoporosis to be a non-serious health condition with negligible impact and perceiving osteoporosis treatments to have a negative risk vs. benefit ratio.[15] Meanwhile, in a study evaluating adherence to oral bisphosphonates in veterans, the most common reason for non-adherence was “I forgot”.[16] Perhaps the intervenable ceiling for persistence is higher than for adherence, for which patient-specific factors such as forgetfulness can be difficult to correct with education and coaching.
Despite this study’s relatively small sample size, depression was found to be highly associated with medication non-adherence at 12 months. Depression has previously been reported to be associated with medication non-adherence in multiple chronic diseases.[17] We were unable to identify any other predictors of non-adherence, likely limited by our sample size. Enrollment percentage was similar between this study and the original C-STOP trial, but this study was not powered to examine multiple covariates.
Real-world medication adherence and persistence is poor, with low rates of adherence and persistence associated with 46% greater risk of fracture.[18] A recent systematic review of nurse-led interventions to promote medication adherence concluded that there is low-quality evidence that some nurse-led interventions may improve medication adherence.[19] In our current resource-strapped healthcare systems, the scale of intervention needs to be balanced with the expected effect size. The summation of this study and the original C-STOP trial would suggest that more resource intensive interventions may not provide greater impact on medication adherence or persistence.
Solving the osteoporosis medication adherence problem is an elusive task. Adherence and persistence rates in this study are higher than those reported in real-world studies. While this study of more intensive CM monitoring and coaching did not achieve our goal of further improving upon the adherence rates achieved by the CM in the original C-STOP study, we feel it is equally important to report these negative results to inform future adherence intervention studies. In a climate of insufficient resources and capacity in most healthcare systems, it is important that further adherence intervention studies balance potential improvements in adherence with intervention cost.
Acknowledgments
The authors would like to thank Jordan Kelly for help in the preparation of this manuscript.
DECLARATIONS
Ethics approval and consent to participate
The current study received ethics approval from the University of Alberta (PRO00018520) and was registered at ClinicalTrials.gov (NCT01401556).
Fig. 1
Flow and outcomes of study participants. BP, bisphosphonate; Ca, calcium supplement; vit D, vitamin D supplement; BMD, bone mineral density.
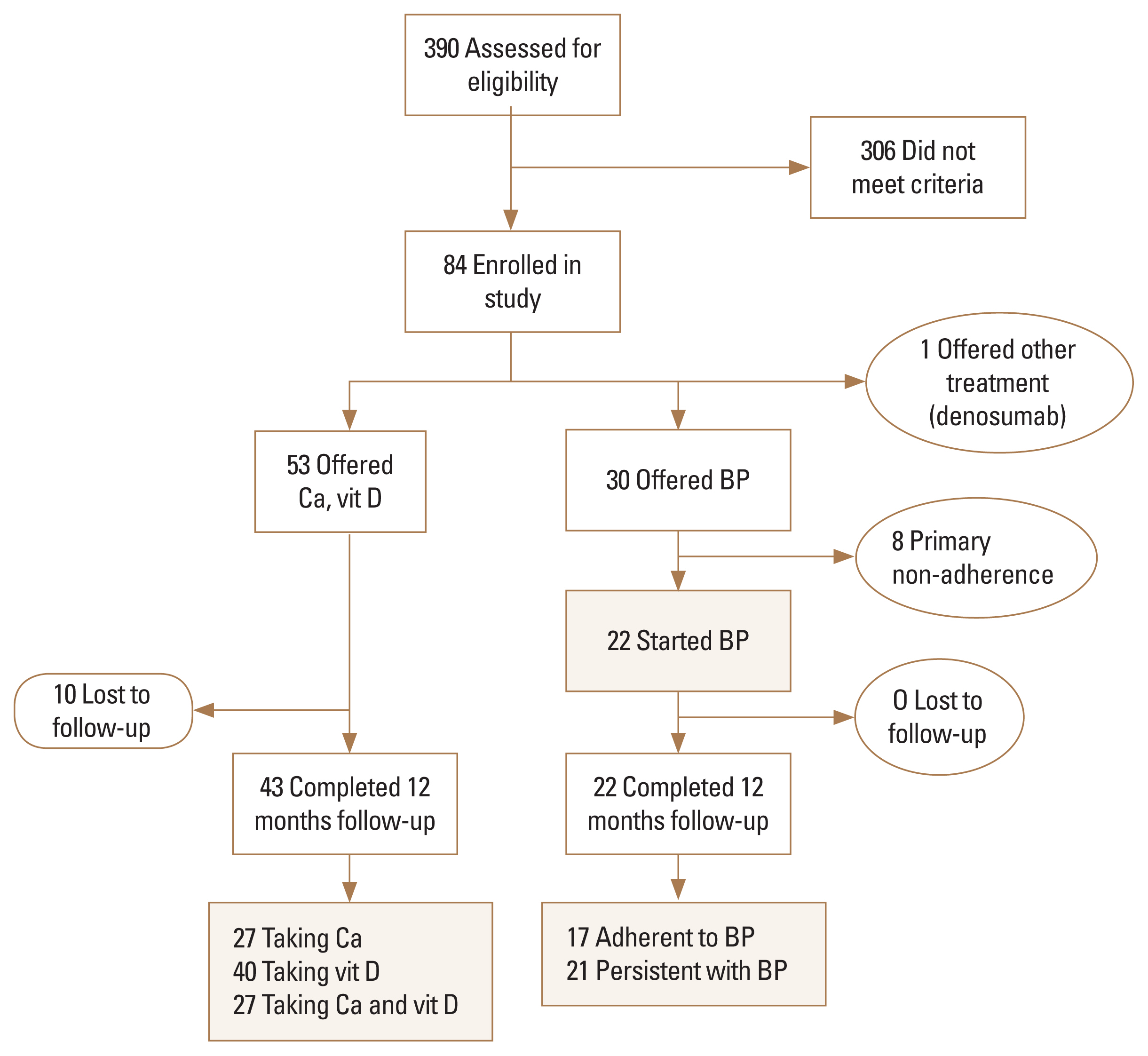
Table 1
Baseline characteristics by 12-month adherence status
REFERENCES
1. International Osteoporosis Foundation. Health professionals 2022 [cited by 2022 Nov 1]. Available from: https://www.osteoporosis.foundation/health-professionals.
2. Langsetmo L, Goltzman D, Kovacs CS, et al. Repeat low-trauma fractures occur frequently among men and women who have osteopenic BMD. J Bone Miner Res 2009;24:1515-22.
https://doi.org/10.1359/jbmr.090319.



3. Kanis JA, Johnell O, De Laet C, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone 2004;35:375-82.
https://doi.org/10.1016/j.bone.2004.03.024.


4. Ye C, Schousboe JT, Morin SN, et al. Time since prior fracture affects mortality at the time of clinical assessment: a registry-based cohort study. Osteoporos Int 2022;33:1257-64.
https://doi.org/10.1007/s00198-021-06236-3.


5. Yeam CT, Chia S, Tan HCC, et al. A systematic review of factors affecting medication adherence among patients with osteoporosis. Osteoporos Int 2018;29:2623-37.
https://doi.org/10.1007/s00198-018-4759-3.


6. Koller G, Goetz V, Vandermeer B, et al. Persistence and adherence to parenteral osteoporosis therapies: a systematic review. Osteoporos Int 2020;31:2093-102.
https://doi.org/10.1007/s00198-020-05507-9.


7. Majumdar SR, McAlister FA, Johnson JA, et al. Comparing strategies targeting osteoporosis to prevent fractures after an upper extremity fracture (C-STOP Trial): a randomized controlled trial. J Bone Miner Res 2018;33:2114-21.
https://doi.org/10.1002/jbmr.3557.


8. Government of Alberta. Edmonton 2022 [cited by 2022 Nov 1]. Available from: https://regionaldashboard.alberta.ca/region/edmonton/#/.
9. McAlister FA, Ye C, Beaupre LA, et al. Adherence to osteoporosis therapy after an upper extremity fracture: a pre-specified substudy of the C-STOP randomized controlled trial. Osteoporos Int 2019;30:127-34.
https://doi.org/10.1007/s00198-018-4702-7.


10. Papaioannou A, Morin S, Cheung AM, et al. 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ 2010;182:1864-73.
https://doi.org/10.1503/cmaj.100771.



11. Armstrong PW, McAlister FA. Searching for adherence: Can we fulfill the promise of evidence-based medicines? J Am Coll Cardiol 2016;68:802-4.
https://doi.org/10.1016/j.jacc.2016.06.006.


12. Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: Terminology and definitions. Value Health 2008;11:44-7.
https://doi.org/10.1111/j.1524-4733.2007.00213.x.


13. Majumdar SR, Johnson JA, McAlister FA, et al. Multifaceted intervention to improve diagnosis and treatment of osteoporosis in patients with recent wrist fracture: a randomized controlled trial. CMAJ 2008;178:569-75.
https://doi.org/10.1503/cmaj.070981.



14. Majumdar SR, Johnson JA, Lier DA, et al. Persistence, reproducibility, and cost-effectiveness of an intervention to improve the quality of osteoporosis care after a fracture of the wrist: results of a controlled trial. Osteoporos Int 2007;18:261-70.
https://doi.org/10.1007/s00198-006-0248-1.


15. Wozniak LA, Johnson JA, McAlister FA, et al. Understanding fragility fracture patients’ decision-making process regarding bisphosphonate treatment. Osteoporos Int 2017;28:219-29.
https://doi.org/10.1007/s00198-016-3693-5.



16. Sagalla N, Lee R, Lyles K, et al. Extent of and reasons for osteoporosis medication non-adherence among veterans and feasibility of a pilot text message reminder intervention. Arch Osteoporos 2021;16:21.
https://doi.org/10.1007/s11657-021-00889-7.



17. Grenard JL, Munjas BA, Adams JL, et al. Depression and medication adherence in the treatment of chronic diseases in the United States: a meta-analysis. J Gen Intern Med 2011;26:1175-82.
https://doi.org/10.1007/s11606-011-1704-y.



18. Imaz I, Zegarra P, González-Enríquez J, et al. Poor bisphosphonate adherence for treatment of osteoporosis increases fracture risk: systematic review and meta-analysis. Osteoporos Int 2010;21:1943-51.
https://doi.org/10.1007/s00198-009-1134-4.


- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,444 View
- 25 Download
- ORCID iDs
-
Carrie Ye

https://orcid.org/0000-0002-9858-5398Finlay A. McAlister

https://orcid.org/0000-0001-7435-3341Debbie Bellerose

https://orcid.org/0009-0008-1085-6087 - Related articles


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



