 |
 |
| jbm > Volume 27(3); 2020 > Article |
|
Abstract
Background
The purpose of this study is to search for reports on the clinical effectiveness of FLS being implemented worldwide through the systematic review, analyze the roles of coordinators in each study, and provide basic data for the development of future coordinator education programs.
Methods
A systematic search of the literature using the Medline, PubMed, and EMBASE databases and the Cochrane Library was conducted for using the following keywords: ‘osteoporosis’ AND ‘fractures’ AND ’secondary prevention’. Finally, 65 studies are included in this study.
Results
At the coordinator-based fracture liaison service (FLS) center, the coordinator (often a nurse) acts as a central player in the establishing of patient connections, orthopedic surgeons, radiologists, and attending physicians. Coordinators help bridge the nursing gap by supporting identification, investigation, initiation of treatment, and patient follow-up. Medics has opened the way to effectively manage patients at high risk of developing another fracture. In addition, nurses are in a unique and important role as nurses responsible for enhancing their daily lives by building relationships with patients and families.
Conclusions
The coordinator in the FLS program plays an important role in the multidisciplinary management of vulnerable fractures, as well as in the diagnosis and treatment of osteoporosis and in maintaining continuity of treatment. In the future, the broader role of coordinators should be systematically organized and developed into accredited educational programs.
Secondary fracture preventions (fracture liaison service [FLS]) including anti-osteoporotic medication and patient education are important for fragility fractured patients because of the high rates of re-fracture after the first fracture [1]. Among fragility fractures including spine, hip, wrist, and proximal humerus, hip fractures are notorious to high mortality, morbidity, and a socioeconomic burden in an aging society. According to recent studies, numbers of fragility fractures are expected to increase trends in the future [2,3]. Secondary fracture prevention programs can be configured in a variety of forms depending on the country's medical system and hospital capacity, and are currently operating in 35 countries around the world [4]. Reported secondary fracture prevention programs can be divided into two main categories. The first is to report the clinical outcomes such as changes in the rate of evaluation and management of osteoporosis or changes in the re-fracture rate after the second fracture prevention program [3,5-7]. The second is proven the economic effect of the second fracture prevention program [8]. Those programs have the same purpose of operation but vary in the way they operate and their members.
Although the management of the secondary fracture prevention program is performed in various ways, the coordinator is important for multidisciplinary management [2]. The role of the coordinator is considering assessment of the past medical history of patients, arrangement of the necessary examinations for osteoporosis, engagement in communication with the primary physician after discharge, and communication among the medical staff in the hospital. They can also help patients to understand the need for osteoporosis evaluation and anti-osteoporotic medication use and to maintain the continuity of patient care. However, there are only a few reports of what role coordinators perform in these secondary fracture prevention programs, and there is no globally recognized training program for them. The hypothesis of this study is that the role and assignment of the coordinator will vary among FLS studies.
Therefore, the purpose of this study is to search for reports on the clinical effectiveness of FLS being implemented worldwide through the systematic review, analyze the roles of coordinators in each study, and provide basic data for the development of future coordinator education programs.
A systematic search of the literature using the Medline, PubMed, and EMBASE databases and the Cochrane Library was conducted for publications (January 2000-October 2019 inclusive) using the following keywords: ‘osteoporosis’ AND ‘fractures’ AND ‘secondary prevention’. The detailed search method is shown in the Supplementary Appendix 1. Relevant papers have also been searched for other local repositories, blogs, and gray literature outlets. The systematic reviews adhere to the Cochrane Collaboration approach.
Inclusion criteria for the trials were: performed in patients ≥50 years of age with all forms of osteoporosis-related fractures; randomized or non-randomized stage 1 to 4 studies; retrospective or prospective observational studies. Excluded are research relating to the prevention of primary fractures or other bone-associated diseases, forms of narrative analyses, systematic reviews, meta-analysis, opinion articles, editorials, case reports, letters, and publications in languages other than English. Two independent reviewers selected the studies by first screening the title and abstract followed by full-text articles. The discrepancy between the 2 reviewers was resolved by consensus or by a third independent reviewer, if necessary. Data analysis used the parameters Population, Procedure, Contrast, Outcomes, Environment (PICOS) and included general information about the article (e.g., authors, publication year), study characteristics (e.g., design, sample size), patient characteristics (e.g., fracture type, osteoporosis duration), and outcomes (bone mineral density testing, treatment initiation, adherence, persistence, rates of re-fracture, and mortality).
Data synthesis and findings were reported in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement. Quality assessments of eligible study methodologies were conducted using the Newcastle - Ottawa scale for non-randomized studies. These 2 authors independently assessed the quality of all studies.
The initial search identified 755 references from the selected databases. The 681 references were excluded by screening the abstracts and titles for duplicates, unrelated articles, case reports, systematic reviews, and non-comparative studies. The remaining 74 studies underwent full-text reviews, and subsequently, nine studies were excluded. Finally, 65 studies are included in this study. The details of the identification of relevant studies are shown in the flow chart of the study selection process (Fig. 1). Seventeen randomized controlled studies, 26 comparative studies, and 22 cohort observation studies were selected for further investigation [1-3,5-7,9-66]. The main characteristics and outcomes of the studies included in this systematic review are presented in Table 1.
Reported studies for second fracture prevention programs were performed in the USA, Canada, and Australia et al. from 2002 to 2017. The most common type of fracture in included studies was hip (57 studies), followed by wrist (43 studies) and humerus (38 studies) fracture.
The most used name of the program was FLS in 18 studies (Table 2). There were also 16 programs containing “intervention”. There were 9 studies involving the expression "integrated" or "multidisciplinary" or "multifaceted". There were also 5 studies that included the expression "fracture prevention" or "secondary prevention".
Coordinator is mentioned in various ways in each study (Table 2). Expression including “nurse” is observed in 20 studies and 11 studies include “coordinator”. In the 6 studies, they were called “manager”, and there were 26 studies that did not mention them. Three studies have also mentioned their real names directly.
There were 31 studies describing the role of the coordinator directly, but 34 studies did not describe the role of the coordinator directly. The described roles of coordinator in included studies can be categorized into 9 roles (Table 3). The most common description is “explaining to the patient the need for osteoporosis evaluation and management” and “identifying the patients to be included in the secondary fracture prevention program” was described in 18 studies. “Casual link with patients” and “patient assessment” are also described as coordinator roles.
The quality assessment for retrospective observational comparison studies using the modified Newcastle-Ottawa Score Tool is measured. All of the included studies were described as observational studies. Sample size calculations were not performed in all studies. The representation of the selected samples was considered appropriate in all included studies. The ascertainment of the assessment tool for sarcopenia was considered as adequate in all observational studies. The response rate, consideration of important confounding factors, ascertainment of assessment tool, and statistical evaluation were reported in all studies. Overall, all of the included individual studies were considered to have a low risk of bias.
In this systematic review, the program of FLS was found to be reported in various forms. There was a model in which patients were screened by pharmacists and evaluated for osteoporosis while a consultation program was provided to the hospitalist or rheumatologist for evaluation and treatment of osteoporosis [20,35,67]. There was also an electronic medical record reminder to increase osteoporosis management in fragility fracture patients [23]. Most of the patients with fractures under the program were older than 50 years of age, but there were programs with inclusion of lower age limits of 40 or 45 years old, and one study had no age limitation [33,51,61,65].
At the coordinator-based FLS center, the coordinator (often a nurse) acts as a central player in the establishing of patient connections, orthopedic surgeons, radiologists, and attending physicians. Coordinators help bridge the nursing gap by supporting identification, investigation, initiation of treatment, and patient follow-up. Medics has opened the way to effectively manage patients at high risk of developing another fracture. In addition, nurses are in a unique and important role as nurses responsible for enhancing their daily lives by building relationships with patients and families.
Based on the results of this systematic review, the role of the FLS coordinator are summarized by explaining the need for osteoporosis evaluation and management, promoting follow-up with primary physicians, recognizing patients, collecting data, evaluating patients, obtaining research approval, casual or daily follow-up, consulting with physicians or transferring information to physicians, coordinating the test. Yuksel et al. [67] reported that osteoporosis assessment was increased, but there were many patients who did not receive appropriate care. For this reason, the authors of these studies attempted to explain the lack of knowledge of the patient and general practitioner, a lack of awareness of current treatment guidelines by both family physicians and orthopedic surgeons, and a perception by orthopedic surgeons. practitioners, poor compliance with prescribed medications and a general lack of communication between all health care providers involved in managing a patient with a fragility fracture. There is a lack of understanding and communication between the patient and the medical staff about this condition, and continuous management of the patient is needed, and this can be done by the coordinator. So, as the results of our study, the most commonly mentioned and important role of the coordinator may be explaining the need for osteoporosis evaluation and management to patients and their families.
Mentions of Coordinator training were observed in 6 studies [17,34,42,44,59,66]. A study by Gardner et al. [42] mentioned that coordinators trained regarding the discussion of the role of osteoporosis in hip fractures, the importance of preventing future fractures, and the effectiveness of currently available therapies. Majumdar et al. [55] stated that the experienced nurse had additional training and expertise in the diagnosis and treatment of osteoporosis. Huntjens et al. [34] described that fracture nurse trained in osteoporosis management and fall risk-assessment [17,34, 42,44]. Mentioned only trained nurses and did not give specific details [59,66].
Although the exact career is not described in many studies, the most commonly mentioned career is a nurse. In terms of medical experience, a nurse may be very suitable for the coordinator and may not require much additional training. Depending on the names of specialist nurses, rheumatology nurse managers, orthopedic nurses, and fracture liaison nurses, you can estimate the major department of nurse affiliation or program operation [22,25,52,58].
In the included studies, the types of fractures for the prevention program also varied. In the study of Kuo et al. [64], all minimal trauma fractures were included, but fractures of finger, toe, and skull were excluded. The subjects of Eekman et al. [46] were similar to that of Kuo’s study, but were excluded facial bone fractures. Because the study of Collinge et al. [51] covers all fracture patients over the age of 18, all fractures in addition to low energy trauma were included in the study. Surely, hip was the most frequently mentioned fracture sites managed by the FLS program. In some studies, vertebral fractures were excluded because they did not increase mortality [5,34]. Hurrington and Lease [50] and Beaton et al. [2] included pelvic fractures in the subjects.
This study has several limitations. First, only limited information could be extracted from these selected papers. Although included studies have reported the role of the FLS coordinator, most studies do not mention detailed protocols of an education program for FLS coordinator. Therefore, it is important to share information on the role of FLS coordinator, and actual educational programs of the FLS coordinator through consensus meetings and academic meeting on different continents. Second, we only included papers that were found after a systematic search against scientific databases. Thus, grey literature on this topic, including abstracts of presentations at meetings on FLS, was not included in this systematic review. Third, we have included retrospective studies, and it may make some biases for data analysis. But, we didn’t perform statistical analysis and just collected for the descriptions of the role of coordination in FLS. Thus, we believe that there are a few possibility for risk of bias by including retrospective studies in our study.
The importance of FLS has been proven in many studies. In addition, it is also reasonable to say that the coordinator is a member who plays a key role in the successful progress of the fracture prevention program between doctors and patients. However, it seems showed that the roles of coordinators and educational programs were not unified worldwide. In our best knowledge, this is the first study for analysis about the roles of coordinator and their education. Based on the results of this study, it is considered that the role of the coordinator should be clearly defined, and efforts should be made to activate the educational program for coordinator training.
In conclusion, the coordinator in the FLS program plays an important role in multidisciplinary management of vulnerable fractures, as well as in the diagnosis and treatment of osteoporosis and in maintaining continuity of treatment. In the future, the broader role of coordinators should be systematically organized and developed into accredited educational programs.
SUPPLMENTARY MATERIAL
Supplementary Appendix 1.
Detailed search strategies for each database. MeSH terms, search terms, and combinations of the 2 were used for each database search
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flow diagram details the process of relevant clinical study selection.
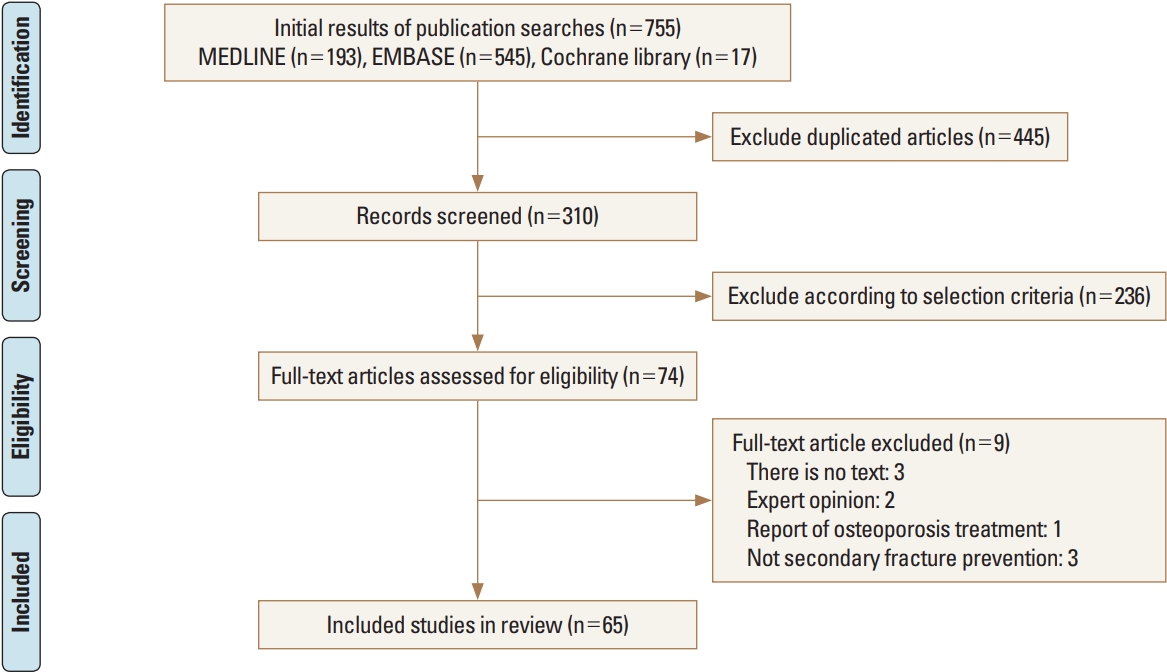
Table 1.
Demographic data of included studies
| Reference | Year | Country | Study design | Age limitation |
Included fracture |
Number of patients | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hip | Vertebra | Wrist | Humerus | Others | ||||||
| Chevalley et al. [49] | 2002 | Switzerland | Cohort observational study | No age limit | Yes | Yes | Yes | Yes | Low trauma fracture | 385 |
| Hawker et al. [33] | 2003 | Canada | Comparative study | >40 | Yes | Yes | Yes | Yes | Ankle | 278 |
| Jachna et al. [20] | 2003 | USA | Comparative study | - | Yes | No | No | No | No | 82 |
| Majumdar et al. [14] | 2004 | Canada | RCT | >50 | No | No | Yes | No | No | 102 |
| Cuddihy et al. [57] | 2004 | USA | Cohort observational study | >45 | No | No | Yes | No | No | 59 |
| Murray et al. [52] | 2005 | UK | Comparative study | >50 | Yes | No | No | Yes | No | 271 |
| Gardner et al. [42] | 2005 | USA | RCT | >65 | Yes | No | No | No | No | 72 |
| Harrington et al. [58] | 2005 | USA | Comparative study | >50 | Yes | Yes | Yes | Yes | Rib, pelvis, long bone | 92 |
| Johnson et al. [38] | 2005 | USA | Comparative study | - | Yes | Yes | Yes | Yes | Patients with history of a fracture | 262 |
| Jones et al. [19] | 2005 | Australia | Comparative study | >70 | Yes | No | No | No | No | 254 |
| Vidán et al. [22] | 2005 | Spain | RCT | >65 | Yes | No | No | No | No | 319 |
| Feldstein et al. [23] | 2006 | USA | RCT | 50-89 | Yes | Yes | Yes | Yes | No | 327 |
| Streeten et al. [40] | 2006 | USA | Comparative study | - | Yes | No | No | No | No | 78 |
| Fisher et al. [54] | 2006 | Australia | Comparative study | >60 | Yes | No | No | No | No | 951 |
| Laslett et al. [37] | 2007 | Australia | Comparative study | >45 | Yes | Yes | Yes | Yes | Low trauma fracture | 121 |
| Davis et al. [31] | 2007 | Canada | RCT | >60 | Yes | No | No | No | No | 48 |
| Majumdar et al. [55] | 2007 | Canada | Comparative study | >50 | No | No | Yes | No | No | 102 |
| Quintos-Macasa et al. [35] | 2007 | USA | Cohort observational study | >54 | Yes | No | No | No | No | 78 |
| Kuo et al. [64] | 2007 | Australia | Cohort observational study | >20 | Yes | Yes | Yes | Yes | Low trauma fracture (no fingers, toes, skull) | 155 |
| Harrington and Lease [50] | 2007 | USA | Cohort observational study | >50 | Yes | Yes | Yes | Yes | Rib, pelvis, long bone | 1,019 |
| Majumdar et al. [55] | 2007 | Canada | RCT | >50 | Yes | No | No | No | No | 220 |
| Cranney et al. [45] | 2008 | Canada | RCT | Postmenopausal women | No | No | Yes | No | No | 261 |
| Majumdar et al. [44] | 2008 | Canada | RCT | >50 | No | No | Yes | No | No | 272 |
| Miki et al. [48] | 2008 | USA | RCT | - | Yes | No | No | No | No | 62 |
| Tosi et al. [9] | 2008 | USA | Comparative study | - | Yes | Yes | Yes | Yes | Low trauma fracture | 635 |
| Collinge et al. [51] | 2008 | USA | Cohort observational study | >18 | Yes | Yes | Yes | Yes | All fracture | 238 |
| Morrish et al. [28] | 2009 | Canada | RCT | >50 | Yes | No | No | No | No | 220 |
| Haaland et al. [12] | 2009 | Canada | Cohort observational study | >50 | Yes | No | No | No | No | 342 |
| Jaglal et al. [17] | 2009 | Canada | Comparative study | >40 | Yes | Yes | Yes | Yes | No | 274 |
| Carpintero et al. [41] | 2009 | Spain | Comparative study | >50 | Yes | Yes | Yes | Yes | Low trauma fracture (no facial bone, skull) | 82 |
| Bessette et al. [7] | 2011 | Canada | RCT | >50 | Yes | Yes | Yes | Yes | Scapula, clavicle, sternum, pelvis, sacrum, proximal and distal tibia, fibula (including ankle), or foot | 1,174 |
| Wallace et al. [25] | 2011 | UK | Comparative study | >75 | Yes | No | No | No | No | 88 |
| Roy et al. [47] | 2011 | USA | Comparative study | - | Yes | No | No | No | No | 140 |
| Lih et al. [65] | 2011 | Australia | RCT | >45 | Yes | No | Yes | Yes | No | 403 |
| Boudou et al. [43] | 2011 | France | Cohort observational study | >50 | Yes | No | Yes | Yes | No | 155 |
| Ojeda-Bruno et al. [63] | 2011 | Spain | Cohort observational study | >50 | Yes | Yes | Yes | Yes | Fragility fracture (no facial bones, skull, ribs, hand, foot) | 380 |
| Huntjens et al. [34] | 2011 | Netherlands | Comparative study | >55 | Yes | No | Yes | Yes | No skull | 3,255 |
| Jaglal et al. [32] | 2012 | Canada | RCT | >40 | Yes | Yes | Yes | Yes | Rib, sternum, pelvis, lower leg, ankle | 267 |
| Leslie et al. [11] | 2012 | Canada | RCT | >50 | Yes | Yes | Yes | Yes | No | 4,264 |
| Heilmann et al. [6] | 2012 | USA | Comparative study | >67 | Yes | Yes | Yes | Yes | Low trauma fracture (no facial bone, skull, fingers, toes) | 1,129 |
| Astrand et al. [60] | 2012 | Sweden | Comparative study | 50-75 | Yes | Yes | Yes | Yes | No | 458 |
| Roux et al. [56] | 2013 | Canada | RCT | >50 | Yes | Yes | Yes | Yes | No | 881 |
| Queally et al. [39] | 2013 | Ireland | Comparative study | Women: >40/ Men: >50 | Yes | Yes | Yes | Yes | Any fracture of osteoporosis on plain radiographs | 61 |
| Chandran et al. [62] | 2013 | Singapore | Cohort observational study | >50 | Yes | Yes | Yes | Yes | No | 287 |
| Goltz et al. [24] | 2013 | Germany | Comparative study | - | - | - | - | - | Osteoporosis fracture | 4,910 |
| Sarfani et al. [10] | 2014 | USA | Cohort observational study | >50 | No | No | Yes | No | No | 151 |
| Van Der Kallen et al. [3] | 2014 | Australia | Comparative study | >50 | Yes | Yes | Yes | Yes | Low trauma fracture | 460 |
| Lee et al. [53] | 2014 | USA | Cohort observational study | >50 | Yes | Yes | Yes | Yes | ICD-9 codes 733.93-733.95, 767.3, 800-829; V54.13 | 444 |
| Ganda et al. [13] | 2014 | Australia | RCT | >45 | Yes | Yes | Yes | Yes | Low trauma fracture | 102 |
| Dehamchia-Rehailia et al. [61] | 2014 | France | Cohort observational study | No age limit | Yes | Yes | Yes | Yes | Low trauma fracture | 335 |
| Huntjens et al. [5] | 2014 | Netherlands | RCT | >50 | Yes | No | Yes | Yes | No | 3,322 |
| Eekman et al. [46] | 2014 | Netherlands | Cohort observational study | >50 | Yes | Yes | Yes | Yes | Low trauma fracture (no facial bone, skull, foot, hand) | 2,207 |
| Ruggiero et al. [29] | 2015 | Italy | Comparative study | >65 | Yes | No | No | No | No | 382 |
| Olenginski et al. [30] | 2015 | USA | Cohort observational study | >50 | Yes | Yes | No | No | No | 1,241 |
| Naranjo et al. [66] | 2015 | Spain | Cohort observational study | >50 | Yes | Yes | Yes | Yes | Low trauma fracture (no facial bone, skull, ribs, hand, foot) | 759 |
| Axelsson et al. [21] | 2016 | Sweden | Comparative study | >50 | Yes | Yes | Yes | Yes | pelvis | 5,329 |
| Amphansap et al. [26] | 2016 | Thailand | Cohort observational study | >50 | Yes | No | No | No | No | 75 |
| Kim et al. [36] | 2016 | New Zealand | Cohort observational study | >50 | Yes | Yes | Yes | Yes | No rib, sternum, clavicle, skull, hand, foot | 301 |
| Shipman et al. [16] | 2016 | UK | Cohort observational study | >50 | Yes | No | Yes | Yes | No | 1,773 |
| Chandran et al. [18] | 2016 | Singapore | Cohort observational study | >50 | Yes | Yes | Yes | Yes | No | 938 |
| Nakayama et al. [27] | 2016 | Australia | Comparative study | >50 | Yes | Yes | Yes | Yes | Low trauma fracture | 931 |
| Beaton et al. [2] | 2017 | Canada | Comparative study | >50 | Yes | Yes | Yes | Yes | Low trauma fracture (pelvis, ankle, other) | 1,130 |
| Cosman et al. [59] | 2017 | USA | Comparative study | >50 | Yes | No | No | No | No | 135 |
| Fraser and Wong [1] | 2017 | Australia | Cohort observational study | >50 | Yes | Yes | Yes | Yes | Low trauma fracture | 166 |
| Henderson et al. [15] | 2017 | Ireland | Cohort observational study | 44-96 | Yes | No | No | No | No | 248 |
Table 2.
Name of fracture liaison services and roles of coordinators in included studies
| Reference | Year | FLS name | Coordinator name | Explaining to need osteoporosis evaluation and management | Encouraging to follow-up with primary physician | Patients identification | Data collection | Patients assessment | Study consent obtain | Casual link or regular follow-up | Discuss with physician or transfer information to physician | Arrangement test | Text about coordinator education |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chevalley et al. [49] | 2002 | Osteoporosis clinical pathway | Coordinator nurse | Yes | No | No | No | No | No | No | No | No | - |
| Hawker et al. [33] | 2003 | Fracture clinic intervention | Coordinator | Yes | Yes | Yes | Yes | Yes | No | No | No | No | - |
| Jachna et al. [20] | 2003 | Hospitalist consultation | - | No | No | No | No | No | No | No | No | No | - |
| Majumdar et al. [14] | 2004 | Intervention | - | No | No | No | No | No | No | No | No | No | - |
| Cuddihy et al. [57] | 2004 | Secondary prevention | Coordinator | Yes | Yes | Yes | No | No | No | Yes | No | Yes | - |
| Murray et al. [52] | 2005 | FLS | Specialist nurse | No | No | No | No | No | No | No | No | No | - |
| Gardner et al. [42] | 2005 | Intervention | Coordinator | No | No | No | No | No | No | No | No | No | Trained regarding the discussion of the role of osteoporosis in hip fractures, the importance of preventing future fractures, and the effectiveness of currently available therapies |
| Harrington et al. [58] | 2005 | Osteoporosis care | Rheumatology nurse man0ager | No | No | No | No | Yes | No | Yes | No | No | - |
| Johnson et al. [38] | 2005 | Intervention | Recruiter | Yes | No | Yes | No | No | Yes | No | No | No | - |
| Jones et al. [19] | 2005 | Fracture protocol | - (person name) | No | No | No | Yes | Yes | No | No | No | No | - |
| Vidán et al. [22] | 2005 | Comprehensive geriatric intervention | Orthopedic nurses | - | No | No | No | No | No | No | No | No | - |
| Feldstein et al. [23] | 2006 | Electronic medical record reminder | - | No | No | No | No | No | No | No | No | No | - |
| Streeten et al. [40] | 2006 | Inpatient consultation | - | No | No | No | No | No | No | No | No | No | - |
| Fisher et al. [54] | 2006 | Geriatric medicine cocare | Orthogeriatric geriatric medicine registrar | No | No | Yes | No | No | No | No | No | No | - |
| Laslett et al. [37] | 2007 | Intervention | - | No | No | No | No | No | No | No | No | No | - |
| Davis et al. [31] | 2007 | Patient empowerment and physician alert intervention | - | No | No | No | No | No | No | No | No | No | - |
| Majumdar et al. [55] | 2007 | Multifaceted intervention | - | No | No | No | No | No | No | No | No | No | - |
| Quintos-Macasa et al. [35] | 2007 | Mandatory rheumatology osteoporosis consultation | - | No | No | No | No | No | No | No | No | No | - |
| Kuo et al. [64] | 2007 | Intervention | - | No | No | No | No | No | No | No | No | No | - |
| Harrington and Lease [50] | 2007 | Osteoporosis care service | Nurse manager | Yes | Yes | No | Yes | No | No | Yes | No | No | - |
| Majumdar et al. [55] | 2007 | Case manager intervention | Osteoporosis case manager | Yes | No | No | No | No | No | No | No | No | - |
| Cranney et al. [45] | 2008 | Multifaceted intervention | Coordinator | No | No | No | No | No | No | No | No | No | - |
| Majumdar et al. [44] | 2008 | Multifaceted intervention | Experienced registered nurse (person name) | Yes | Yes | No | No | No | Yes | No | No | No | Experienced registered nurse who had additional training and expertise in the diagnosis and treatment of osteoporosis |
| Miki et al. [48] | 2008 | Inpatient osteoporosis evaluation | - | No | No | No | No | No | No | No | No | No | - |
| Tosi et al. [9] | 2008 | FLS | Nurse practitioner | No | No | No | No | No | No | No | No | No | - |
| Collinge et al. [51] | 2008 | Osteoporosis Protocol | Nurse clinician | Yes | No | Yes | No | No | No | Yes | No | No | - |
| Morrish et al. [28] | 2009 | Case manager intervention | Case manager | No | No | No | No | No | No | No | No | Yes | - |
| Haaland et al. [12] | 2009 | Fracture think osteoporosis program | - | No | No | No | No | No | No | No | No | No | - |
| Jaglal et al. [17] | 2009 | Educational intervention | Coordinator | Yes | Yes | No | No | No | No | Yes | Yes | No | Trained to carry out the educational outreach visits according to the principles outlined |
| Carpintero et al. [41] | 2009 | Prevent project | - | No | No | No | No | No | No | No | No | No | - |
| Bessette et al. [7] | 2011 | Educational interventions | - | No | No | No | No | No | No | No | No | No | - |
| Wallace et al. [25] | 2011 | FLS | Fracture liaison nurse | No | No | No | No | Yes | No | No | Yes | Yes | - |
| Roy et al. [47] | 2011 | Hospitalist-orthopaedic surgeon integrated model of care | - | No | No | No | No | No | No | No | No | No | - |
| Lih et al. [65] | 2011 | Targeted intervention | Investigator | No | No | No | Yes | Yes | No | No | No | No | - |
| Boudou et al. [43] | 2011 | FLS | Nurse | No | No | Yes | No | No | No | No | No | No | - |
| Ojeda-Bruno et al. [63] | 2011 | Secondary prevention program | - | No | No | No | No | No | No | No | No | No | - |
| Huntjens et al. [34] | 2011 | FLS | Fracture nurse | Yes | Yes | No | No | Yes | No | No | No | No | Trained in osteoporosis management and fall risk-assessment |
| Jaglal et al. [32] | 2012 | Multidisciplinary osteoporosis program | Coordinator | Yes | Yes | No | Yes | Yes | Yes | No | No | No | - |
| Leslie et al. [11] | 2012 | Intervention | - | No | No | No | No | No | No | No | No | No | - |
| Heilmann et al. [6] | 2012 | Clinical-pharmacy-based osteoporosis management service | Primary care clinical pharmacy specialist | No | No | No | No | No | No | Yes | Yes | No | - |
| Astrand et al. [60] | 2012 | Osteoporosis screening program | Nurse and secretary | No | No | No | No | No | No | No | No | No | - |
| Roux et al. [56] | 2013 | Integrated multidisciplinary approach | Coordinator | Yes | Yes | No | No | No | No | Yes | No | No | - |
| Queally et al. [39] | 2013 | Screening for osteoporosis in a community fracture clinic setting | - | No | No | No | No | No | No | No | No | No | - |
| Chandran et al. [62] | 2013 | FLS | Case manager (specialist nurse) | No | No | Yes | No | No | No | No | No | No | - |
| Goltz et al. [24] | 2013 | Program of integrated care | - | No | No | No | No | No | No | No | No | No | - |
| Sarfani et al. [10] | 2014 | Integrated model of care | Patient educator | Yes | No | Yes | No | No | Yes | No | No | No | - |
| Van Der Kallen et al. [3] | 2014 | Fracture prevention service | Fracture prevention nurse | Yes | No | No | No | Yes | No | Yes | No | No | - |
| Lee et al. [53] | 2014 | Osteoporosis electronic consult service | - | No | No | No | No | No | No | No | No | No | - |
| Ganda et al. [13] | 2014 | FLS | - | No | No | No | No | No | No | No | No | No | - |
| Dehamchia-Rehailia et al. [61] | 2014 | FLS | FLS nurse | No | No | Yes | No | No | No | No | No | No | - |
| Huntjens et al. [5] | 2014 | FLS | Fracture nurse | Yes | No | Yes | No | No | No | No | No | No | - |
| Eekman et al. [46] | 2014 | FLS | Fracture nurse | Yes | No | Yes | No | Yes | No | No | No | No | - |
| Ruggiero et al. [29] | 2015 | Fracture prevention service (multidisciplinary integrated model of care) | - | Yes | No | No | No | No | No | Yes | No | No | - |
| Olenginski et al. [30] | 2015 | High-risk osteoporosis clinic: improving osteoporosis and post-fracture care with an organized, programmatic approach | Clinical nurse specialists or nurse manager | No | No | No | No | No | No | No | No | No | - |
| Naranjo et al. [66] | 2015 | FLS | Nurse | No | No | No | No | Yes | No | No | No | No | Trained nurse |
| Axelsson et al. [21] | 2016 | FLS | Coordinator | No | No | No | No | No | No | No | No | No | - |
| Amphansap et al. [26] | 2016 | FLS | - | No | No | No | No | No | No | No | No | No | - |
| Kim et al. [36] | 2016 | FLS | FLS coordinator | Yes | No | Yes | No | No | No | No | No | No | - |
| Shipman et al. [16] | 2016 | FLS | - | No | No | No | No | No | No | No | No | No | - |
| Chandran et al. [18] | 2016 | FLS | - | No | No | No | No | No | No | No | No | No | - |
| Nakayama et al. [27] | 2016 | FLS | - | No | No | No | No | No | No | No | No | No | - |
| Beaton et al. [2] | 2017 | Fragility fracture screening program | Coordinator | No | No | Yes | No | No | No | No | No | No | - |
| Cosman et al. [59] | 2017 | FLS | Geriatric NP (person name) | No | No | No | No | No | No | No | No | No | Well-trained geriatric NP |
| Fraser and Wong [1] | 2017 | Secondary fracture prevention | Fracture liaison coordinator | No | No | Yes | No | No | No | No | No | No | - |
| Henderson et al. [15] | 2017 | Orthogeriatric service | - | No | No | No | No | No | No | No | No | No | - |
Table 3.
Roles of coordinator in included studies
REFERENCES
1. Fraser S, Wong PK. Secondary fracture prevention needs to happen in the country too: the first two and a half years of the Coffs Fracture Prevention Clinic. Aust J Rural Health 2017;25:28-33.


2. Beaton DE, Vidmar M, Pitzul KB, et al. Addition of a fracture risk assessment to a coordinator’s role improved treatment rates within 6 months of screening in a fragility fracture screening program. Osteoporos Int 2017;28:863-9.



3. Van der Kallen J, Giles M, Cooper K, et al. A fracture prevention service reduces further fractures two years after incident minimal trauma fracture. Int J Rheum Dis 2014;17:195-203.


4. International Osteoporosis Foundation. FLS around the world apply for Capture the Fracture® recognition. 2020 [cited by 2020 Apr 1]. Available from: https://www.capturethefracture.org/fls-around-world-apply-capture-fracture%C2%AE-recognition.
5. Huntjens KM, van Geel TA, van den Bergh JP, et al. Fracture liaison service: impact on subsequent nonvertebral fracture incidence and mortality. J Bone Joint Surg Am 2014;96:e29.


6. Heilmann RM, Friesleben CR, Billups SJ. Impact of a pharmacist-directed intervention in postmenopausal women after fracture. Am J Health Syst Pharm 2012;69:504-9.



7. Bessette L, Davison KS, Jean S, et al. The impact of two educational interventions on osteoporosis diagnosis and treatment after fragility fracture: a population-based randomized controlled trial. Osteoporos Int 2011;22:2963-72.


8. Major G, Ling R, Searles A, et al. The costs of confronting osteoporosis: Cost study of an Australian fracture liaison service. JBMR Plus 2019;3:56-63.


9. Tosi LL, Gliklich R, Kannan K, et al. The American Orthopaedic Association’s “own the bone” initiative to prevent secondary fractures. J Bone Joint Surg Am 2008;90:163-73.

10. Sarfani S, Scrabeck T, Kearns AE, et al. Clinical efficacy of a fragility care program in distal radius fracture patients. J Hand Surg Am 2014;39:664-9.


11. Leslie WD, LaBine L, Klassen P, et al. Closing the gap in postfracture care at the population level: a randomized controlled trial. CMAJ 2012;184:290-6.



12. Haaland DA, Cohen DR, Kennedy CC, et al. Closing the osteoporosis care gap: increased osteoporosis awareness among geriatrics and rehabilitation teams. BMC Geriatr 2009;9:28.




13. Ganda K, Schaffer A, Pearson S, et al. Compliance and persistence to oral bisphosphonate therapy following initiation within a secondary fracture prevention program: a randomised controlled trial of specialist vs. non-specialist management. Osteoporos Int 2014;25:1345-55.



14. Majumdar SR, Rowe BH, Folk D, et al. A controlled trial to increase detection and treatment of osteoporosis in older patients with a wrist fracture. Ann Intern Med 2004;141:366-73.


15. Henderson CY, Shanahan E, Butler A, et al. Dedicated orthogeriatric service reduces hip fracture mortality. Ir J Med Sci 2017;186:179-84.



16. Shipman KE, Stammers J, Doyle A, et al. Delivering a quality-assured fracture liaison service in a UK teaching hospital-is it achievable? Osteoporos Int 2016;27:3049-56.


17. Jaglal SB, Hawker G, Bansod V, et al. A demonstration project of a multi-component educational intervention to improve integrated post-fracture osteoporosis care in five rural communities in Ontario, Canada. Osteoporos Int 2009;20:265-74.



18. Chandran M, Cheen M, Ying H, et al. Dropping the ball and falling off the care wagon. Factors correlating with nonadherence to secondary fracture prevention programs. J Clin Densitom 2016;19:117-24.


19. Jones G, Warr S, Francis E, et al. The effect of a fracture protocol on hospital prescriptions after minimal trauma fractured neck of the femur: a retrospective audit. Osteoporos Int 2005;16:1277-80.



20. Jachna CM, Whittle J, Lukert B, et al. Effect of hospitalist consultation on treatment of osteoporosis in hip fracture patients. Osteoporos Int 2003;14:665-71.


21. Axelsson KF, Jacobsson R, Lund D, et al. Effectiveness of a minimal resource fracture liaison service. Osteoporos Int 2016;27:3165-75.




22. Vidán M, Serra JA, Moreno C, et al. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc 2005;53:1476-82.


23. Feldstein A, Elmer PJ, Smith DH, et al. Electronic medical record reminder improves osteoporosis management after a fracture: a randomized, controlled trial. J Am Geriatr Soc 2006;54:450-7.


24. Goltz L, Degenhardt G, Maywald U, et al. Evaluation of a program of integrated care to reduce recurrent osteoporotic fractures. Pharmacoepidemiol Drug Saf 2013;22:263-70.


25. Wallace I, Callachand F, Elliott J, et al. An evaluation of an enhanced fracture liaison service as the optimal model for secondary prevention of osteoporosis. JRSM Short Rep 2011;2:8.



26. Amphansap T, Stitkitti N, Dumrongwanich P. Evaluation of police general hospital’s fracture liaison service (PGH’s FLS): the first study of a fracture liaison service in Thailand. Osteoporos Sarcopenia 2016;2:238-43.

27. Nakayama A, Major G, Holliday E, et al. Evidence of effectiveness of a fracture liaison service to reduce the re-fracture rate. Osteoporos Int 2016;27:873-9.


28. Morrish DW, Beaupre LA, Bell NR, et al. Facilitated bone mineral density testing versus hospital-based case management to improve osteoporosis treatment for hip fracture patients: additional results from a randomized trial. Arthritis Rheum 2009;61:209-15.


29. Ruggiero C, Zampi E, Rinonapoli G, et al. Fracture prevention service to bridge the osteoporosis care gap. Clin Interv Aging 2015;10:1035-42.


30. Olenginski TP, Maloney-Saxon G, Matzko CK, et al. High-risk osteoporosis clinic (HiROC): improving osteoporosis and postfracture care with an organized, programmatic approach. Osteoporos Int 2015;26:801-10.



31. Davis JC, Guy P, Ashe MC, et al. HipWatch: osteoporosis investigation and treatment after a hip fracture: a 6-month randomized controlled trial. J Gerontol A Biol Sci Med Sci 2007;62:888-91.



32. Jaglal SB, Donescu OS, Bansod V, et al. Impact of a centralized osteoporosis coordinator on post-fracture osteoporosis management: a cluster randomized trial. Osteoporos Int 2012;23:87-95.


33. Hawker G, Ridout R, Ricupero M, et al. The impact of a simple fracture clinic intervention in improving the diagnosis and treatment of osteoporosis in fragility fracture patients. Osteoporos Int 2003;14:171-8.



34. Huntjens KM, van Geel TC, Geusens PP, et al. Impact of guideline implementation by a fracture nurse on subsequent fractures and mortality in patients presenting with non-vertebral fractures. Injury 2011;42 Suppl 4:S39-43.


35. Quintos-Macasa AM, Quinet R, Spady M, et al. Implementation of a mandatory rheumatology osteoporosis consultation in patients with low-impact hip fracture. J Clin Rheumatol 2007;13:70-2.


36. Kim D, Mackenzie D, Cutfield R. Implementation of fracture liaison service in a New Zealand public hospital: Waitemata district health board experience. N Z Med J 2016;129:50-5.
37. Laslett LL, Whitham JN, Gibb C, et al. Improving diagnosis and treatment of osteoporosis: evaluation of a clinical pathway for low trauma fractures. Arch Osteoporos 2007;2:1-6.



38. Johnson SL, Petkov VI, Williams MI, et al. Improving osteoporosis management in patients with fractures. Osteoporos Int 2005;16:1079-85.



39. Queally JM, Kiernan C, Shaikh M, et al. Initiation of osteoporosis assessment in the fracture clinic results in improved osteoporosis management: a randomised controlled trial. Osteoporos Int 2013;24:1089-94.



40. Streeten EA, Mohamed A, Gandhi A, et al. The inpatient consultation approach to osteoporosis treatment in patients with a fracture. Is automatic consultation needed? J Bone Joint Surg Am 2006;88:1968-74.

41. Carpintero P, Gil-Garay E, Hernández-Vaquero D, et al. Interventions to improve inpatient osteoporosis management following first osteoporotic fracture: the PREVENT project. Arch Orthop Trauma Surg 2009;129:245-50.



42. Gardner MJ, Brophy RH, Demetrakopoulos D, et al. Interventions to improve osteoporosis treatment following hip fracture. A prospective, randomized trial. J Bone Joint Surg Am 2005;87:3-7.

43. Boudou L, Gerbay B, Chopin F, et al. Management of osteoporosis in fracture liaison service associated with long-term adherence to treatment. Osteoporos Int 2011;22:2099-106.



44. Majumdar SR, Johnson JA, McAlister FA, et al. Multifaceted intervention to improve diagnosis and treatment of osteoporosis in patients with recent wrist fracture: a randomized controlled trial. CMAJ 2008;178:569-75.

45. Cranney A, Lam M, Ruhland L, et al. A multifaceted intervention to improve treatment of osteoporosis in postmenopausal women with wrist fractures: a cluster randomized trial. Osteoporos Int 2008;19:1733-40.



46. Eekman DA, van Helden SH, Huisman AM, et al. Optimizing fracture prevention: the fracture liaison service, an observational study. Osteoporos Int 2014;25:701-9.



47. Roy A, Heckman MG, O’Connor MI. Optimizing screening for osteoporosis in patients with fragility hip fracture. Clin Orthop Relat Res 2011;469:1925-30.



48. Miki RA, Oetgen ME, Kirk J, et al. Orthopaedic management improves the rate of early osteoporosis treatment after hip fracture. A randomized clinical trial. J Bone Joint Surg Am 2008;90:2346-53.


49. Chevalley T, Hoffmeyer P, Bonjour JP, et al. An osteoporosis clinical pathway for the medical management of patients with low-trauma fracture. Osteoporos Int 2002;13:450-5.



50. Harrington JT, Lease J. Osteoporosis disease management for fragility fracture patients: new understandings based on three years' experience with an osteoporosis care service. Arthritis Rheum 2007;57:1502-6.


51. Collinge C, LeBus G, Gardner MJ, et al. Osteoporosis in orthopaedic trauma patients: a diagnosis and treatment protocol. J Orthop Trauma 2008;22:541-7.


52. Murray AW, McQuillan C, Kennon B, et al. Osteoporosis risk assessment and treatment intervention after hip or shoulder fracture. A comparison of two centres in the United Kingdom. Injury 2005;36:1080-4.


53. Lee RH, Lyles KW, Pearson M, et al. Osteoporosis screening and treatment among veterans with recent fracture after implementation of an electronic consult service. Calcif Tissue Int 2014;94:659-64.




54. Fisher AA, Davis MW, Rubenach SE, et al. Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J Orthop Trauma 2006;20:172-8.


55. Majumdar SR, Johnson JA, Lier DA, et al. Persistence, reproducibility, and cost-effectiveness of an intervention to improve the quality of osteoporosis care after a fracture of the wrist: results of a controlled trial. Osteoporos Int 2007;18:261-70.


56. Roux S, Beaulieu M, Beaulieu MC, et al. Priming primary care physicians to treat osteoporosis after a fragility fracture: an integrated multidisciplinary approach. J Rheumatol 2013;40:703-11.


57. Cuddihy MT, Amadio PC, Gabriel SE, et al. A prospective clinical practice intervention to improve osteoporosis management following distal forearm fracture. Osteoporos Int 2004;15:695-700.



58. Harrington JT, Barash HL, Day S, et al. Redesigning the care of fragility fracture patients to improve osteoporosis management: a health care improvement project. Arthritis Rheum 2005;53:198-204.


59. Cosman F, Nicpon K, Nieves JW. Results of a fracture liaison service on hip fracture patients in an open healthcare system. Aging Clin Exp Res 2017;29:331-4.



60. Astrand J, Nilsson J, Thorngren KG. Screening for osteoporosis reduced new fracture incidence by almost half: a 6-year follow-up of 592 fracture patients from an osteoporosis screening program. Acta Orthop 2012;83:661-5.



61. Dehamchia-Rehailia N, Ursu D, Henry-Desailly I, et al. Secondary prevention of osteoporotic fractures: evaluation of the Amiens University Hospital's fracture liaison service between January 2010 and December 2011. Osteoporos Int 2014;25:2409-16.



62. Chandran M, Tan MZ, Cheen M, et al. Secondary prevention of osteoporotic fractures--an “OPTIMAL” model of care from Singapore. Osteoporos Int 2013;24:2809-17.



63. Ojeda-Bruno S, Naranjo A, Francisco-Hernández F, et al. Secondary prevention program for osteoporotic fractures and long-term adherence to bisphosphonates. Osteoporos Int 2011;22:1821-8.



64. Kuo I, Ong C, Simmons L, et al. Successful direct intervention for osteoporosis in patients with minimal trauma fractures. Osteoporos Int 2007;18:1633-9.



65. Lih A, Nandapalan H, Kim M, et al. Targeted intervention reduces refracture rates in patients with incident non-vertebral osteoporotic fractures: a 4-year prospective controlled study. Osteoporos Int 2011;22:849-58.



- TOOLS
-
METRICS

-
- 5 Crossref
- 0 Scopus
- 5,563 View
- 183 Download
- ORCID iDs
-
Yong Han Cha

https://orcid.org/0000-0002-7616-6694Yong-Chan Ha

https://orcid.org/0000-0002-6249-0581Ki-Soo Park

https://orcid.org/0000-0001-5571-3639Jun-Il Yoo

https://orcid.org/0000-0002-3575-4123 - Related articles


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Supplement
Supplement Print
Print



