INTRODUCTION
Cushing's syndrome is involved in several clinical symptoms including fatigability, weakness, amenorrhea, truncal obesity, hirsutism, edema, hypertension, diabetes, and osteoporosis. Cushing's syndrome is known as an important cause of secondary osteoporosis and it is often accompanied by fractures. Glucocorticoid influences more on osteoblastic cells than the osteoclasts and also alters secretion of gonadotropin and calcium absorption, thereby occurring bone loss. It affects more on trabecular bones rather than cortical bones. Reduction of bone mineral density (BMD) is exhibited in children or young women and vertebral fractures may occur before diagnosis. A case has been reported that a lumbar compression fracture was observed domestically in a 32 year old female patient with Cushing's syndrome.[1] However, it is rare to diagnose Cushing's syndrome with repetitive pathologic fractures occurring in young women. The authors described a case that Cushing's syndrome caused by adrenal adenoma was diagnosed in a 26 year old woman who visited our hospital due to repetitive multiple pathologic fractures. Since the fractures occurred after the removal of functioning adrenal adenoma, the patient was treated with parathyroid hormone.
CASE
Sacrum of the 28 year old female patient were fractured while moving an object seven months before visiting a hospital so she received conservative treatment. Two months before visiting the hospital, thoracic vertebra radiography was performed since she claimed lower back pain. Compression fractures were diagnosed on 12th thoracic vertebra and then she visited orthopedics in our hospital. A dual energy X-ray absorptiometry (DXA) of lumbar spine and femur revealed relatively low BMD for her age and she was referred to endocrinology department for further investigation. There was no medication history of taking calcium, vitamin D supplement, and oriental medicine etc. Menarche was began when she was 13 years old but menstruation was stopped one year before the hospital visit; but there was no unusual finding in obstetrics examination so she was still being monitored. There was no alcohol drinking and smoking history, family history of osteoporosis and fractures, and other unusual findings.
At the time of her visiting, she complained severe back to pain and had 154.4 cm of height, 45.2 kg of body weight, 19 kg/m2 of body mass index (BMI), 130/100 mmHg of blood pressure, 87 times/minute of pulse, 18 times/minute of breathing, and 36.9℃ of body temperature. Moon face was not clearly shown but mild edema on the face and truncal obesity. The upper and bottom limbs were relatively thin and skin became thin as well. Purple spots were exhibited.
A blood test, leukocyte, hemoglobin, platelets were 7,630 mm3 (neutrophils 84.7%, lymphocyte 8.7%, eosinocyte 0.3%), 13.4 g/dL, 169,000/µL. Fasting glucose, albumin, aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, and creatinine were 112 mg/dL, 4.1 g/dL, 19 IU/L, 27 IU/L, 409 IU/L, and 0.8 mg/dL, respectively. Total calcium and phosphate were 9.1 mg/dL and 2.7 mg/dL, respectively, and albumin/globulin ratio was not reversed. In addition, serum intact parathyroid hormone, osteocalcin, C-telopeptide, and concentration of plasma 25-hydroxy vitamin D were 36.43 pg/mL (normal range: 13-54), 5 ng/mL (normal range: 4-20), 0.83 ng/mL (normal range: < 0.573), and 33.18 ng/mL, respectively. Thyroid function tests resulted in free T4 1.3 ng/dL, thyroid stimulating hormone (TSH) 0.43 mIU/L, and T3 57.2 ng/dL, indicating a normal range.
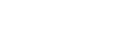
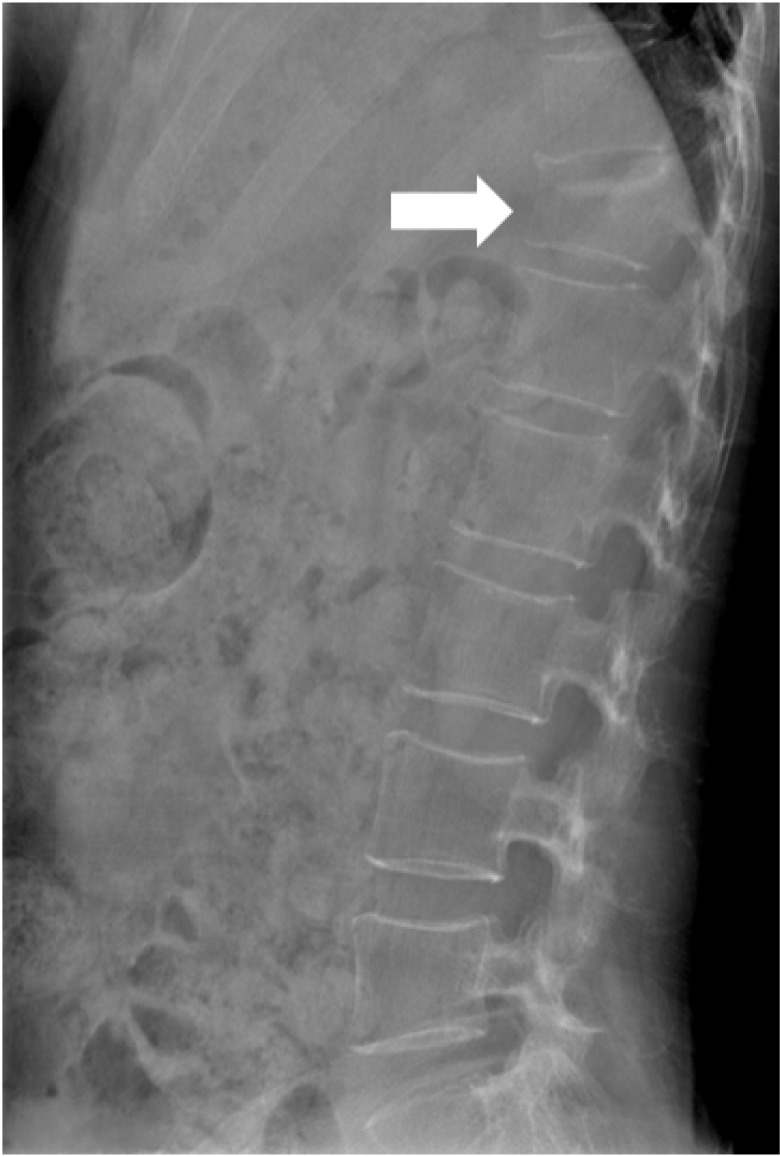
A compression fracture were observed at 12th thoracic vertebra in spine x-ray (Fig. 1) and Z-score of lumbar vertebrae (L1-4) and femoral neck were -2.9 and -2.1 on DXA, respectively, representing below the expected range for age (Fig. 2).
While being hospitalized, the patient put on brace for conservative treatment with regards to the vertebral compression fracture. As the patient claimed chest pain during the treatment, plain radiography was performed. In the result, fractures were exhibited at right 7th and 10th ribs. Cushing's syndrome was considered due to repetitive pathologic fractures, low BMD regarding age, and the gross findings. Then, free cortisol in urine and 17-hydroxycorticosteroid were tested and then resulted 1,062 µg/day and 17.3 mg/day (normal range: 3-15), respectively, indicating cortisol excess. In order to confirm the diagnosis, a low-dose dexamethasone suppression test was carried out. As a result, we confirmed diagnosis of Cushing's syndrome because basal cortisol was 29.34 µg/dL and cortisol on 3rd day was 28.40 µg/dL indicating that it was not suppressed. Since adrenocorticotrophic hormone was relatively low (10.26 pg/mL), abdomen computed tomography (CT) was performed without a high-dose dexamethasone suppression test considering Cushing's syndrome caused by adrenal adenoma. A 2.7 × 2.4 sized adenoma was observed on left adrenal gland (Fig. 3), so that the patient received laparoscopic left adreanalectomy and was given 30 mg of hydrocortisone a day after the operation. However, after 2 months, the patient visited the hospital again due to severe pain on the lower back again and new compression fractures were taken place at 6th, 8th, 9th, and 11th thoracic vertebrae and 2th and 3rd lumbar vertebrae. Then, 750 mg of calcium citrate and 10 µg of cholecalciferol were given once a day and 20 µg of 1-34 parathyroid hormone (teriparatide) was injected once a day for 6 months total. In DXA performed 11 months after the treatment, BMD of lumbar vertebrae (L1-4) and femoral neck were increased by 4.5%, 1.9%, and 5.5%, respectively. Serum alkaline phosphatase, intact parathyroid hormone, osteocalcin, and concentration of blood 25-hydroxyl vitamin D were 304 IU/L, 28.57 pg/mL (normal range: 13-54), 16.1 ng/mL (normal range: 4-20), and 21.5 ng/mL, respectively. Currently, hydrocortisone was reduced to 10 mg a day; the patient is still being monitored without further fracture occurrences.
DISCUSSION
Although Cushing's syndrome shows typical clinical aspects caused by excessive secretion of cortisol, sometimes classic findings were not expressed at the same time and biochemical markers showed various patterns, indicating that it can be difficult to diagnose Cushing's syndrome clinically.[2] Since Cushing's syndrome is also diagnosed in young women, like the present case, tests for secondary osteoporosis including Cushing's syndrome should be performed in cases where multiple pathologic fractures with unclear causes were occurred in young women. In the present case, even if a moon-like face and truncal obesity were not clearly shown, tests with regards to Cushing's syndrome were performed since there were purple spots on her skin and compression fractures at 12th thoracic vertebra.
Fractures occur in 30-50% of Cushing's syndrome patients, especially in thoracic vertebrae and lumbar vertebrae. Moreover, osteoporosis occurs in 50% of Cushing's syndrome patients.[3] and bone loss is occurred more frequent in Cushing's syndrome caused by adrenal tumors, like the present case, than that of in Cushing's syndrome caused by pituitary tumors.[4]
Trabecular bones are influenced more affected by glucocorticoid than cortical bones. As a result, vertebral and rib fractures are commonly observed in patients with Cushing's syndrome or long-term steroid administration.[5] However, fractures can also occur on long bones rarely as well as pelvic bones. The fractures induce lower back pain, kyphosis, and reduction in height and then these further induce new fractures again. In the patients with Cushing's syndrome, glucocorticoid induces muscle weakness of lower extremities by protein catabolism so that these further induce injury from a fall and fractures. Bones are stimulated by strong muscle contraction itself. When the muscle is weak, bone loss is accelerated by diminishing the stimulation on bones.[3]
Although there are multiple mechanisms regarding the bone loss in Cushing's syndrome, the most important mechanism for the glucocorticoid excess induced bone loss, is the dysfunction and decrease in numbers of osteoblast. The exact mechanism is to be elucidated but it has been suggested that glucocorticoid inhibits the proliferation and genesis of osteoblast, and induces apoptosis of osteoblast thereby decreasing the numbers of osteoblast. In addition, as glucocorticoid suppresses the synthesis of bone proteins such as osteocalcin, alkaline phosphatase activity, as well as formation of type 1 collagen, it is found that osteoblast related osteocalcin and alkaline phosphatase activity were lowered in Cushing's syndrome patients.[3] In present case, unexpectedly, the alkaline phosphatase activity was found to be elevated and this might be because of multiple vertebral fractures; osteocalcin was decreased while C-terminal telopeptide (CTx) was increased in the patient. Further, regardless of vitamin D, the intestinal absorption as well as reabsorption of calcium from the renal tubules was inhibited in the hypercortisolism.[3] This increases the parathyroid hormone secretion and affects bone metabolism. However, glucocorticoid induced osteoporosis was exhibited somewhat differently compared to the one found in primary hyperparathyroidism. In the glucocorticoid induced osteoporosis, trabecular bones are more affected than cortical bones and the bone turnover is relatively slow whereas loss in cortical bones is found rather than trabecular bones with high bone turnover in primary hyperparathyroidism.[6] Third mechanism is that since glucocorticoid affects on the activity as well as production of growth factors and hormones that regulates bone and calcium metabolism. The hypercortisolism inhibits the growth hormones and insulin like growth factor that stimulate bone formation, decreases gonadotropin thereby decreasing the BMD.[7] In present case, secondary amenorrhea was observed while menstruation was initiated after the normalization of cortisol, indicating that changes in sex hormones are partially affecting BMD.
Decreases in BMD of the lumbar vertebrae are found earlier than that of peripheral skeletal in Cushing's syndrome patients. The trabecular bone tissues exhibit fast bone turnover and higher glucocorticoid sensitivity than cortical bones thereby occurring bone loss faster. Thus, all Cushing's syndrome patients should be examined for BMD of the lumbar vertebrae. However, one thing should be noted is that a person administered with glucocorticoid represents higher fractures rate than the one without glucocorticoid if the BMD is comparable.[3] Similarly, frequent vertebral compression fractures were observed in the case considering the BMD of the patient.
Faggiano et al.[8] monitored 36 patients who were fully cured from Cushing's syndrome for 3.9 years average; loss in trabecular bones, vertebral fractures, and scoliosis were significantly increased compared to the control group and there was a significant correlation between the numbers of vertebral fractures, and disease duration, age when the disease is initiated and the urinary free cortisol level when diagnosed. These indicate the likelihood of vertebrae damage prior to the full recovery of bone metabolism from Cushing's syndrome; therefore, appropriate treatment as well as regular radiological monitoring, including vertebrae should be accompanied when treating Cushing's syndrome patients, particularly for the patients with difficulties in normalizing cortisol level.
Osteoporosis due to the glucocorticoid is reversible. Although there are no clear changes in BMD after 6 months from the complete cure of Cushing's syndrome, osteoblast effects are ameliorated with elevated osteocalcin; thus, most patients exhibit the recovered BMD within 12-36 months after the level of cortisol is normalized.[3] Manning et al.[9] confirmed that the BMD of the lumbar vertebrae and femoral neck was normalized in 17 patients who are completely cured from Cushing's syndrome. Although the exact mechanisms regarding the recovery of BMD are to be elucidated, it might be due to 1) remaining structure that may generate new bones by osteoblast since sponge tissues were reserved even though trabecular bones got thinner 2) the recovery of the osteocalcin level after the treatment of hypercortisolism.[2] Increments in bone mass occur very slowly and it normally takes 10 years to be completely recovered. Thus, there are multiple studies addressing that utilizing anti-resorptive drugs would be effective prior to the complete recovery since such patients have more chances in fractures. Di Somma C et al.[10] reported that the BMD was improved better compared to the control group, when alendronate was given after the surgical treatment of Cushing's syndrome; further authors recommended the bisphosphonate treatment would be effective to prevent additional bone loss if there is continued hypercortisolism after the surgical treatment. However, further investigations with regard to the long term administration, are warranted given the mechanisms of bisphosphonate that may inhibit osteogenesis, observed in steroid induced osteoporosis. Therefore, the use of parathyroid hormone that increase bone formation is recommendable.[5] So far, there is no large randomized study has been done with regard to the parathyroid hormone treatment for Cushing's syndrome patients; there are several studies done in glucocorticoid induced osteoporosis patients.
If menopausal women with glucocorticoid induced osteoporosis were daily received with parathyroid hormone for 1 year, BMD was improved on vertebrae compared to that of the control group.[11] In addition, when the group with daily administration of 10 mg alendronate and the group with 20 µg of parathyroid hormone treatment per day were compared, significant increment of BMD along with less fractures were found in the group with parathyroid hormone at 6th and 12th month.[12]
In this case, repetitive fractures were observed in the middle and even after the hospitalization for the adrenal adenoma excision; it was difficult to wait the natural increases in bone mass due to such high fracture risk. Thus, parathyroid hormone has been administrated for 6 months and discontinued for further monitoring. Although the BMD was measured after 5 months from the time point when the drug was withdrawn, due to patient's circumstances, better and higher BMD were observed compared to the natural recovery as previously reported in other studies.
CONCLUSION
Repetitive pathologic fractures in young female are very rare and the possibility of secondary osteoporosis should be considered in such cases. The patient visited the hospital owing to the repetitive fractures and was examined for endocrine function tests and was diagnosed as Cushing's syndrome via adrenal adenoma. Later, there were repetitive fractures after adrenal adenoma were removed so that parathyroid hormone treatment was given. Since then, increased BMD was observed and the patient is being monitored without additional fractures.


 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






