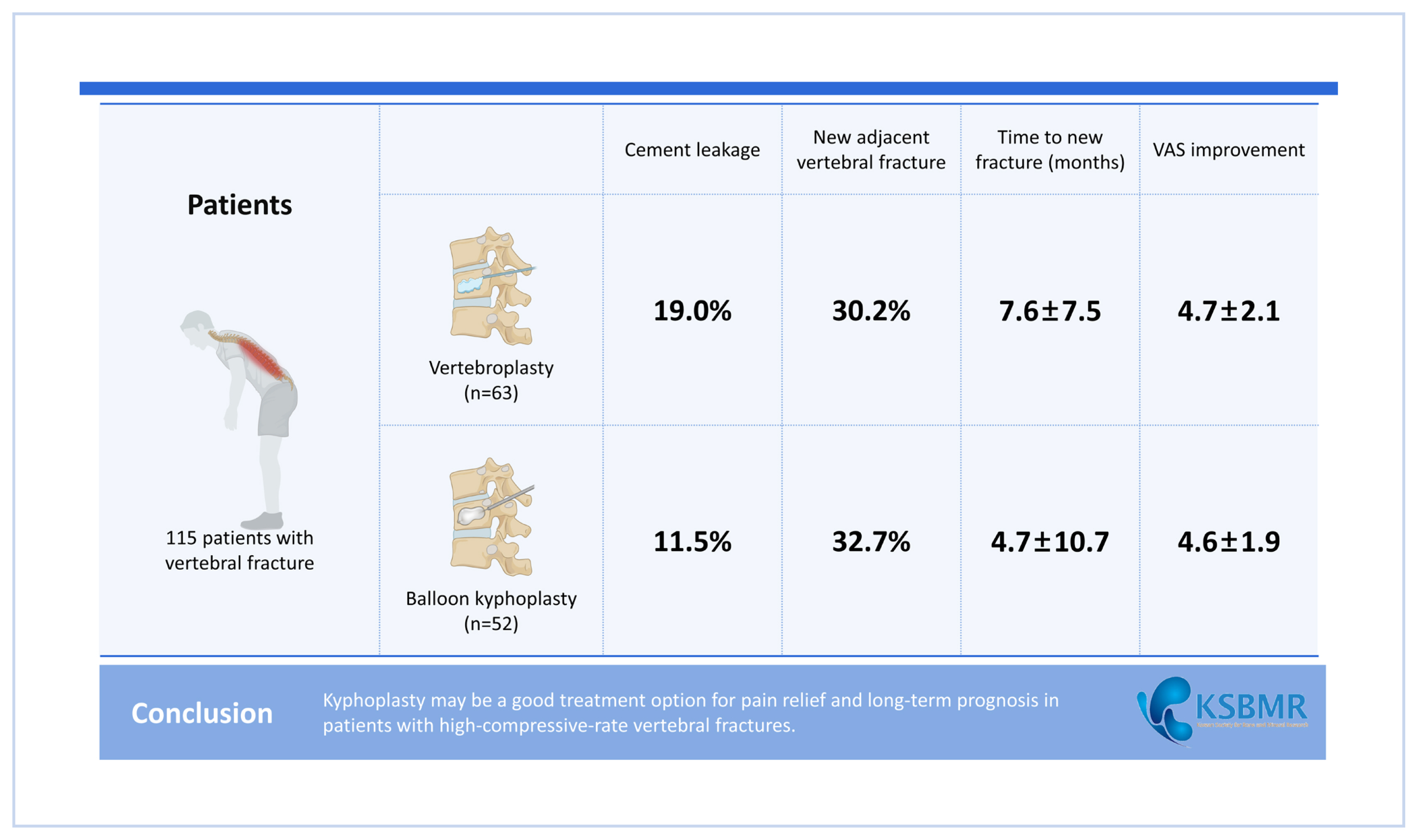
Comparison of Clinical and Radiological Outcomes after Vertebroplasty and Balloon Kyphoplasty in the Treatment of Osteoporotic Vertebral Compression Fractures
Article information
Abstract
Background
Vertebroplasty (VP) and balloon kyphoplasty (KP) are effective means with which to improve pain and function in osteoporotic vertebral compression fractures. However, the risk of complications after these procedures is poorly understood, with concerns regarding adjacent vertebral fractures. This study retrospectively investigated the clinical and radiological outcomes of these procedures.
Methods
A total of 115 patients who experienced their first vertebral fracture were treated with VP (N=63) or KP (N=52) at the Dankook University Hospital between January 2013 and December 2022. The clinical outcomes were evaluated using the visual analog scale (VAS) preoperative and at 1-year follow-up. Radiological comparisons were performed for kyphosis correction, vertebral height restoration, and postoperative cement leakage.
Results
KP was more effective than VP, especially for vertebral body height restoration and kyphotic angle reduction (P<0.05). However, the incidence of cement leakage, new adjacent vertebral fractures, and improvement in pain assessed by VAS did not differ statistically between the 2 groups (P>0.05).
Conclusions
Considering that KP was performed on fractures with severe deformity, no differences were observed in the clinical outcomes and incidence of adjacent vertebral fractures compared Considering that KP was performed for fractures with severe deformity, there was no difference in clinical outcomes and incidence of adjacent vertebral fractures compared to VP. Improvements in radiological measurements were demonstrated. Therefore, KP may be a good treatment option for pain relief and long-term prognosis in patients with high-compressive-rate vertebral fractures.
INTRODUCTION
Osteoporotic vertebral compression fractures (VCFs) have a high incidence and have direct and indirect negative consequences on health-related quality of life in elderly patients and costs to the healthcare system.[1,2] Currently, percutaneous vertebroplasty (VP) and balloon kyphoplasty (KP) are widely used in clinical practice. Both procedures are minimally invasive procedure that provides pain relief and stability by correcting kyphosis and body height in patients with osteoporotic compression fractures.[3–5] KP is a minimally invasive intervention method that utilizes an inflatable balloon to create space in the central portion of the vertebral body before cement injection, aiming to restore height as an alternative to VP.[6] One of the main concerns in these procedures is that augmentation with bone cement can lead to the development of new fracture at untreated levels and extravasation of inserted cement.[7–9] In our previous study, we obtained research results indicating that a higher rate of height restoration in the vertebral body is associated with an increased risk of adjacent vertebral fractures.[10] Therefore, we were concerned about the possibility of complications occurring after KP, particularly when performing excessive kyphotic angle correction in cases of significant deformity. So, in this study, we investigated retrospectively the risk of complications comparing radiological and clinical outcomes 1 year after the procedures between VP and KP performed over 10 years period at our institute to evaluate the safety and efficiency of KP.
METHODS
1. Patients
Between January 2013 and December 2022, 396 cases of 368 patients with minor trauma or non-traumatic painful osteoporotic VCF were treated with VP (297 cases) or KP (99 cases) at the Dankook University Hospital. Patients with underlying diseases (metastatic diseases, infection, end-stage renal disease and tumor; hemangioma) other than benign osteoporotic compression fracture were excluded from the study. Retrospectively, we included patients of similar age who experienced their first vertebral fracture and were followed up for more than 1 year after the procedure. Consequently, the study was conducted on 115 patients (63 VPs and 52 KPs).
2. Procedures
In our institute, VP and KP were performed by 1 experienced spine surgeon. Patients were followed up at 1, 3, 6 months post-operation and yearly on an outpatient basis for clinical evaluation and radiological examination.
3. Radiographic examinations
All measurements of vertebral body height and kyphotic angle taken using plain radiographs before and after surgery were undertaken by one of the authors. We choose the standardized method recommended by McKiernan et al. [11] to report vertebral height. For calculations, the pre-fracture height of the vertebral body was assumed to be equal to the average of the adjacent vertebral heights, and the pre- and post-procedure heights were expressed as a percentage of the estimated normal height. We used local kyphotic angle to assess the degree of wedge deformation of the fractured vertebral body and the Cobb technique to calculate the segmental kyphotic angle across the fractured level and the measurement was taken from the superior endplate of the vertebra one level above the treated vertebra to the inferior endplate of the vertebral body one level below the treated vertebra (Fig. 1, 2).[12]
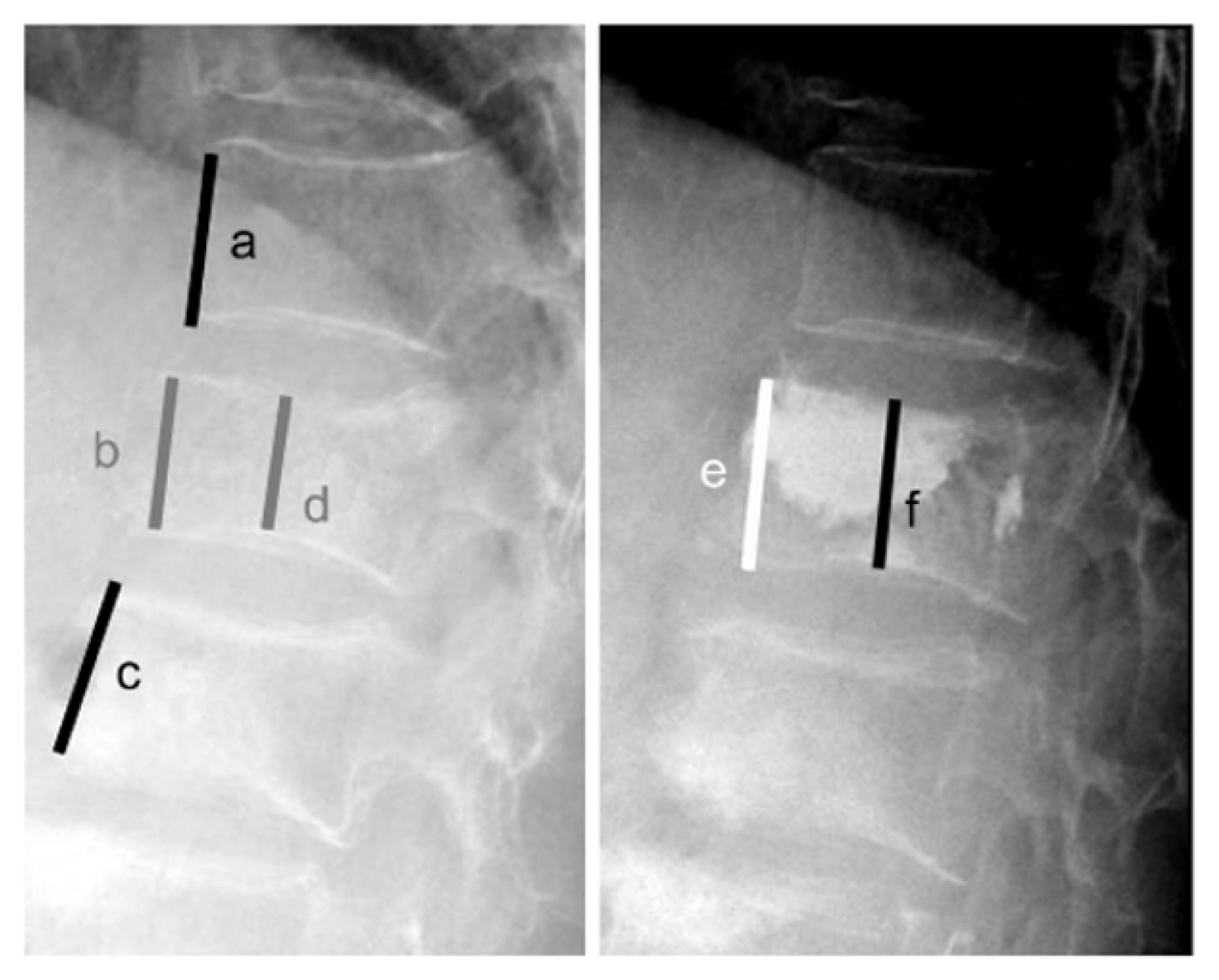
The method used for determining vertebral body height restoration rate. Vertebral body height before compression fracture (Y): Y=(a +c)/2. Anterior height restoration (A): A=[(e-b)/Y]×100 (%). Middle height restoration (M): M=[(f-d)/Y]×100 (%).
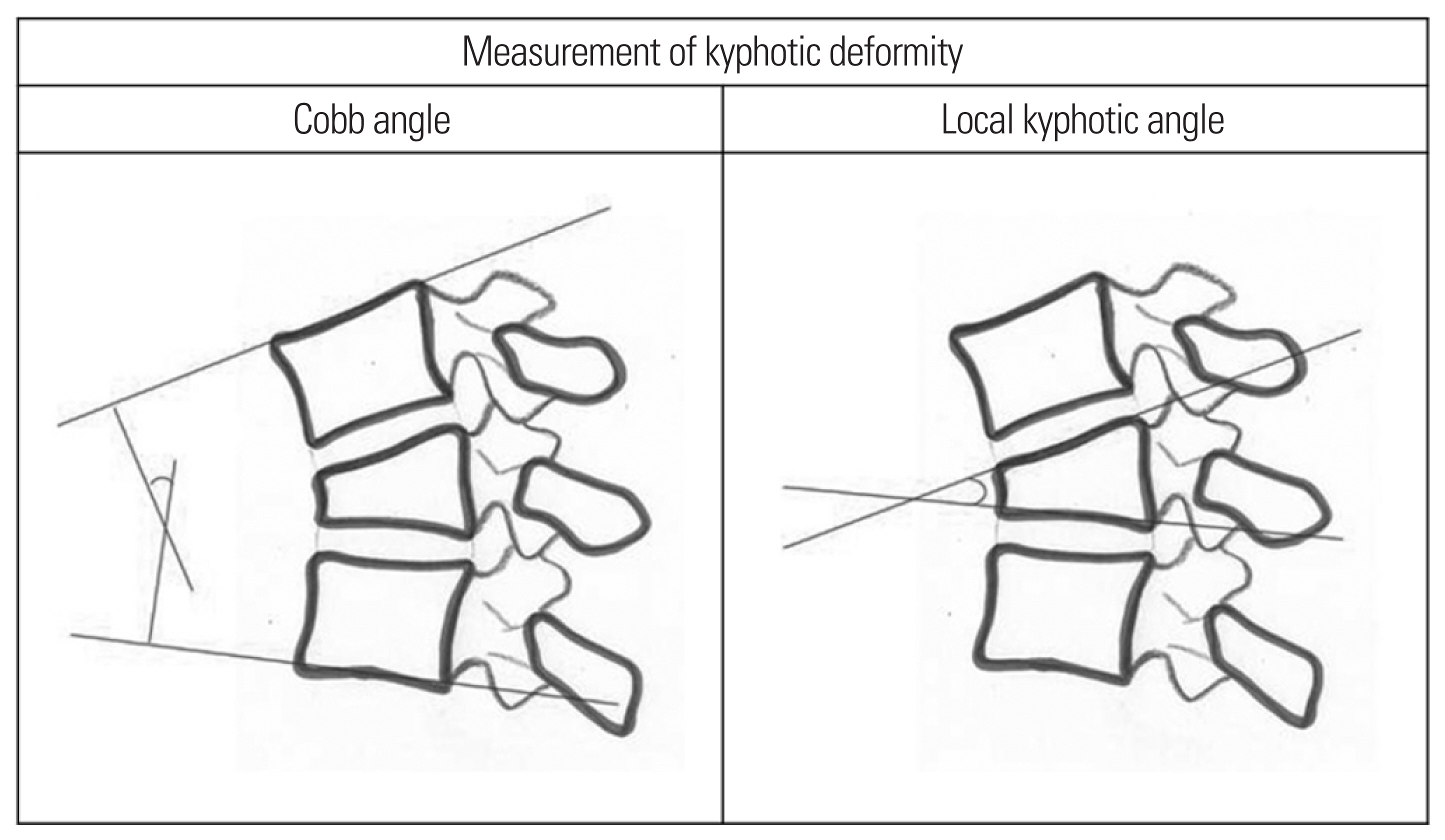
The method used for determining vertebral Cobb angle and local kyphotic angle. Cobb angle is the degree of superior endplate of the vertebra one level above the treated vertebra to inferior endplate of the vertebral body one level below the treated vertebra. Local kyphotic angle is the degree of superior endplate to inferior endplate of treated vertebra.
Review of patient data
To consider possible predictors of new vertebral body fractures, we investigated age, gender, method chosen for percutaneous augmentation, amount of cement injected per vertebral body (cement volume), extravasation of cement to intervertebral disc space (cement leakage), and bone mineral density (BMD). According to the site of fracture occurrence, we categorized the cases into the thoracic spine, T–L junction (T12 and L1 spine), or lumbar spine groups. Clinical outcomes were assessed using visual analog scale (VAS) measured before surgery and at each outpatient visit; at 1, 3, 6 months and yearly.
4. Statistical analysis
Age, BMD, cement volume, VAS, extra vertebral cement leakage, the restoration rates of anterior vertebral heights, and local and kyphotic angle differences were recorded. Baseline comparisons were performed using the t-test, Mann-Whitney U test, and χ2 test. SPSS statistics (version 27.0; SPSS Inc., Chicago, IL, USA) was used for all statistical analyses, and P-values of less than 0.05 were deemed significant.
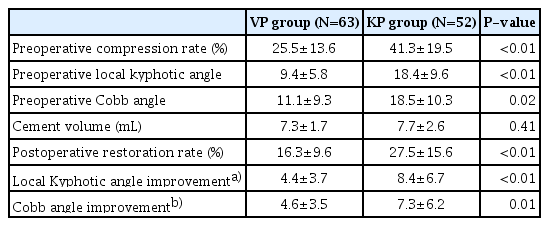
RESULTS
A total of 115 patients managed with VP and KP were enrolled in this study. They consisted of 63 (54.8%) patients in the VP group and 52 (45.2%) in the KP group. Mean age of VP group was 80.2 (68–95) and 74.2 (65–84) in KP group. The level of fracture was distributed between T6 and L4 spine and was most prevalent on the thoracolumbar junction. There was no significant difference between 2 groups for demographic data statistically including BMD which mostly corresponds to osteoporosis (Table 1).

Comparison of demographic and baseline characteristics between patients treated with vertebroplasty and patients treated with kyphoplasty
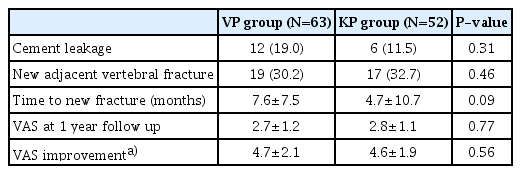
There was a significant difference in the mean preoperative vertebral body height, local wedge angle and adjacent kyphotic angle (Cobb angle) between the VP and KP groups, respectively (P<0.01). Although the mean volume of polymethylmethacrylate (PMMA) cement per body was not different in both groups (7.3±1.7 mL vs. 7.7±2.6 mL, in the VP and KP group; P=0.41), the restoration rate, degrees of improvement local kyphotic angle and cobb angle were significantly higher after KP as compared with VP (P<0.05) (Table 2). The rate of cement leakage cases was higher in the VP group (19.0%) than in the KP group (11.5%), but a statistically significant difference could not be confirmed (P=0.31). Between the 2 groups, a significant difference in the change of pre- and postoperative restoration rate and 2 angle measurements, but no difference was observed in the incidence of adjacent fractures (P=0.46). Comparing the period of occurrence of adjacent fractures in the 2 groups, it was found that fractures occurred in a relatively short period in the KP group, but there was no statistical significance (P=0.09). At 1 year follow-up, significant improvements in pain evaluated by VAS were shown but there were no statistically significant differences (P=0.56) when comparing the VAS scores between the 2 groups (Table 3).
DISCUSSION
Patients suffering from compression vertebral fracture will have developed irreversible spinal deformity (kyphosis) associated with several significant health consequences including decreased physical functioning and diminished health-related quality of life,[13,14] increased future fracture risk,[1,15] impaired balance, and increased incidence of falls.[16]
There is still controversy in studies as to whether new vertebral body fractures are a result of the natural progression of osteoporosis or a consequence of augmentation.[17] But restoration of vertebral height and sagittal balance through the interventions is believed to be important in the treatment of long-term increased morbidity and mortality that arises from compression fractures and spinal deformity.[13] A cost-effectiveness study conducted in the United States concluded that both procedures were more cost-effective than conservative treatment,[18] and Svedbom et al. [17] in the United Kingdom argued that KP was more cost-effective than VP.
Several studies have reported that treated fracture transfers excessive load to the surrounding vertebral body due to the biomechanical effect of PMMA cement injected with KP or VP, increasing the risk of adjacent vertebral fractures.[1,4] Kim et al. [9] found an increased risk of new adjacent fracture to level with increased height restoration after vertebral augmentation. For the risk factors for peripheral fractures, biomechanical studies and results suggest that the greater the height and angle resilience, the more fractures there are. Based on this findings, because of the greater degree of height recovery with the KP procedure, new fractures can be expected to be more common after KP.[19]
However, this was not the result found in this study. Same as in our study, Wang et al. [20] concluded that both interventions were considered to have similar risks with subsequent fracture and cement leakage. Ma et al. [21] conducted a meta-analysis that encompassed 12 studies with 1,081 patients, and there were no statistical differences in VAS, Oswestry Disability Index (ODI), cement leakage rates, and adjacent vertebral fracture rates. Zhao et al. [22] also represented both VP and KP showed similar effects on short-term pain relief, posterior vertebral body mass, and adjacent-level fractures.
Rho et al. [23] and Lin et al. [24] reported that leakage of cement into the intervertebral disc during augmenting vertebrae with bone cement increases the risk of new fractures of adjacent vertebral bodies. Komemushi et al. [25] also determined the only independent variable associated with fractures was cement leakage into the intervertebral disc. Based on indirect comparison of KP and VP case series, previous systematic reviews or meta-analyses showed that KP appears to have a substantially lower incidence of cement leakage than VP.[26–28] and it had been suggested that cement leaks into the adjacent intervertebral disc space affect the mechanical loading of either the disc or adjacent vertebrae, which might predispose the patient to an adjacent-level fracture.[25]
As expected, our study proved the advantage of KP in the correction of vertebral deformity associated with VCFs of severe deformity (Table 3). KP is an alternative minimally invasive intervention method for VP that uses an expandable balloon to restore height and create space in the central part of the vertebral body before cement injection.[19] Data from our study showed that KP was performed in a group of patients with severe preoperative deformity and showed significantly better angle recovery rates (Table 3). In our previous study, We confirmed that the frequency of complications decreased when additional pain control was provided through nerve root blocks.[29] Also, considering the impact of sagittal balance on the patient’s long-term pain, gait, quality of life, and risk of falling, KP is considered to be a very useful treatment.[13,15] Evaluation is limited as there have been no studies on the long-term results of pain, radiological and clinical complications, but short-term results showed no significant difference from VP.
This was a retrospective study, so there was a lack of randomization for both groups of patients and a relatively short follow-up period. Although we treated many patients at a single institution for 10 years, we unable to obtain a numerous long-term follow-up patient group. As the long-term outcome after the procedure could not be confirmed, the impact of osteoporosis treatment could not be studied. It is believed that randomized controlled trials with larger sample sizes, multicenter studies, and longer follow-up data are needed to complement the current results and confirm more accurate results.
Considering that KP was performed on fractures with severe deformity, it didn’t make a difference in clinical outcomes and incidence of adjacent vertebral fractures compared to VP and improvements in radiological measurement have been demonstrated. As improvement in kyphotic deformity can impact a prolonged patient’s physical activity and pain, KP may be a good treatment choice for pain improvement and long-term prognosis in high compressive rate vertebral fracture.
Notes
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Dankook University Hospital, College of Medicine, Dankook University.
Conflict of interest
No potential conflict of interest relevant to this article was reported.