Seasonal Variations and Common Places of Hip Fractures in Elderly Patients: Nine Year Consecutive Survey
Article information
Abstract
Background
Fall prevention is important for reducing hip fractures. The aim of this study was to determine the relationship between variables related to hip fractures according to sex and season.
Methods
This study included patients admitted for fragility hip fractures between 2012 and 2021. Patients were interviewed by a junior resident before discharge. Data on sex, age, diagnosis, osteoporosis treatment, direction, voiding problems, ambulatory function, seasons, weather, time of day, place, location, floor condition, activity during fall, and perceived reason for fall were collected and analyzed.
Results
A total of 1,118 patients were included (279 males and 839 females). In both sexes, indoor falls were prevalent throughout all seasons, but males showed a higher proportion of outdoor falls, especially in winter during cloudy or snowy weather. Rooms and walking were the most common locations and activities during falls. The poor ambulatory function was associated with a higher prevalence of indoor falls. Osteoporosis treatment rates were low and did not differ according to Koval stage. Winter was associated with higher osteoporosis non-treatment group. Urgency/incontinence in female patients caused a higher proportion of falls during the evening time.
Conclusions
Strategies for indoor fall prevention and vigilant osteoporosis diagnosis and treatment are important for all seasons, especially for frail elderly patients. Outdoor fall prevention emphasized for male patients, and education around nighttime falls should be provided for female patients with voiding dysfunction.
INTRODUCTION
Hip fracture in the elderly results in high morbidity and mortality. One-year mortality after hip fracture is 8.4% to 36%, which is higher than community living control population,[1] and about 50% of patients after hip fracture lose their level of ambulation [2] and lose independence,[3] which results in high costs to society.[4,5]
For the prevention of hip fractures, fall prevention is important as falls are responsible for 98% of hip fractures,[6] and as such, fall prevention initiatives are becoming an important part of community health care, with an increasing aging population, alongside diagnosis and treatment of osteoporosis.[4] However, compared to osteoporosis treatment, fall prevention programs have been largely inconclusive for hip fractures until now.[7,8]
Several intrinsic and extrinsic factors are known to be risk factors for falls. Intrinsic factors related to hip fracture are advancing age, history of previous falls, muscle weakness, gait and balance problems, poor vision, and chronic diseases such as arthritis.[9] Extrinsic factors related to hip fracture are lack of handrails, poor lighting, slippery or uneven surfaces, use of walking aids and poor footwear.[10]
However, the fall prevention interventions done in previous studies showed reduction in fall rate, but not in fall related morbidity and mortality and fall related hospitalization. Thus the correlation of intrinsic and extrinsic factors related in falls resulting in hip fracture itself should be a focus of study, not the fall itself. Thus, we aimed to investigate the relationship of intrinsic and extrinsic factors related to falls which resulted in hip fracture.
METHODS
1. Study population
Between November 2012 and October 2021, patients aged >65 who were admitted for surgery due to acute hip fracture including femoral neck, intertrochanteric and subtrochanteric fractures after falls were eligible for this study. Pathologic fracture including atypical fracture and bedridden patients were excluded. During this period, 1,162 patients visited our hospital due to a hip fracture. Of these patients, 44 patients could not undergo interview due to 23 refusal and 21 poor interview results. As a result, data on 1,118 patients were analyzed for this study.
2. Interview and data collection
Eligible patients were identified at the time of admission and information was prospectively collected by a junior resident from the patient and/or family member before discharge. Detailed information on fall information was prospectively collected. Collected intrinsic factors related to falls resulting in hip fracture were sex, age, diagnosis (femoral neck fracture, intertrochanteric fracture, subtrochanteric fracture), osteoporosis treatment (yes or no), direction of all (anterior, side and posterior), voiding problem (no problem, frequency, urgency, incontinence, dysuria, and end-stage renal disease) and ambulatory function (Koval grade [11]). Collected extrinsic factors related to falls resulting in hip fracture were season (Spring [March, April, May], Summer [June, July, August], Autumn [September, October, November] and Winter [December, January, February]), weather (fine, cloud, rain, snow), time of day (dawn [12:01 AM to 06:00 AM], morning [06:01 AM to 12:00 PM], afternoon [12:01 PM to 06:00 PM], evening [06:01 PM to 12:00 AM]), place of fall (indoors, outdoors), location of fall (Room, Living Room, Toilet, Kitchen, Balcony, Front Door, Yard, Stairs, Side walk, Road, Others), floor condition (Linoleum, Tile, Wood, Soil, Cement, Aspalt, Ice, Others), activity during fall (walking, standing, stairs [up], stairs [down], wheelchair, exercise, walking aid, chair, bed, carrying objects, changing position, and others) and perceived reason of fall (slippage, trip over, false step, collision, dizziness, fall from chair/bed, standing).
3. Statistical analysis
Analysis were performed to determine whether there were significant differences in hip fracture occurrence regarding sex, season, location and activity. Additionally, we tried to evaluate whether there is some relationship between ambulatory function, voiding problems, and osteoporosis treatment. Continuous variables were reported as mean±standard deviation. For comparison, ANOVA was used for continuous variables and post hoc analysis was done with least significant difference. A χ2 test was used for categorical variables. SPSS for Windows statistical package (version 27.0; SPSS Inc., Chicago, IL, USA) was used, and a P-value of less than 0.05 was considered significant.
RESULTS
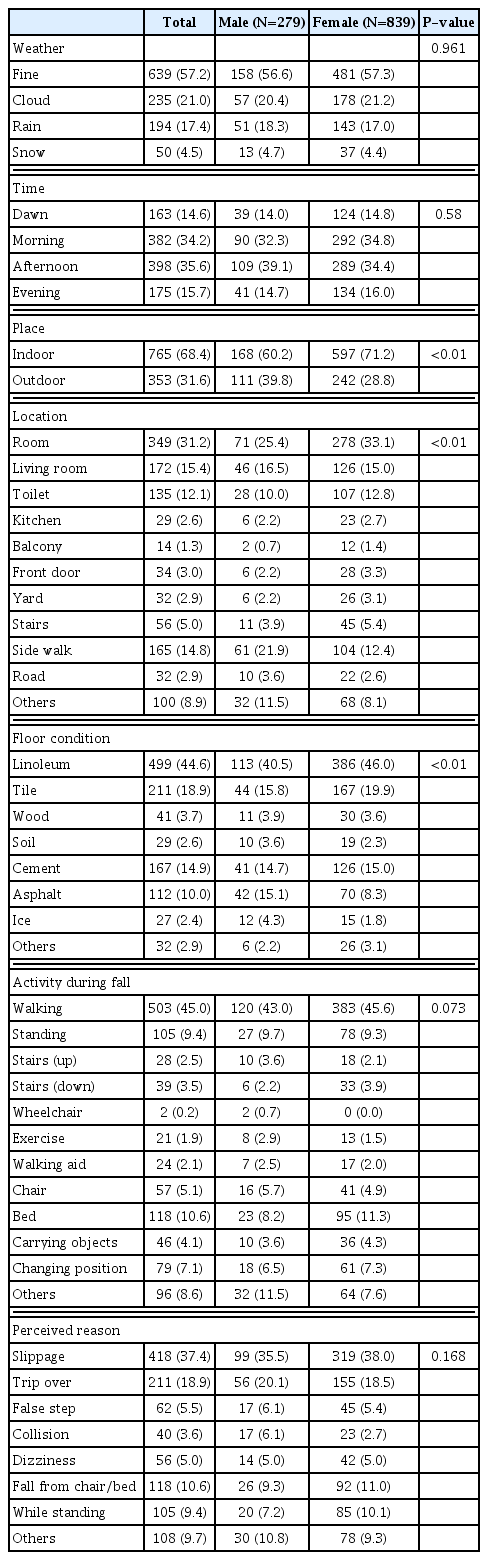
Of the 1118 patients, 279 (25.0%) were male and 839 (75.0%) were female. The diagnosis was 509 femoral neck fractures (45.5%), 572 intertrochanteric fractures (51.2%), and 37 subtrochanteric fractures (3.3%). The side was the most common direction of fall (56.8%) followed by posterior (32.8%) and anterior (10.4%). The 21.3% of patients received osteoporosis treatment (Table 1). Among weather, fine weather was the most common (57.2%) and most fractures occurred in the morning (34.2%) and afternoon (35.6%). Place of fall was indoor in 68.4%, and most common location of fall was room (31.2%) and most common condition of floor was linoleum (44.6%). Walking was the most common activity during falls (45.0%), and slippage was the most common perceived reason for falls (37.4%) (Table 2).
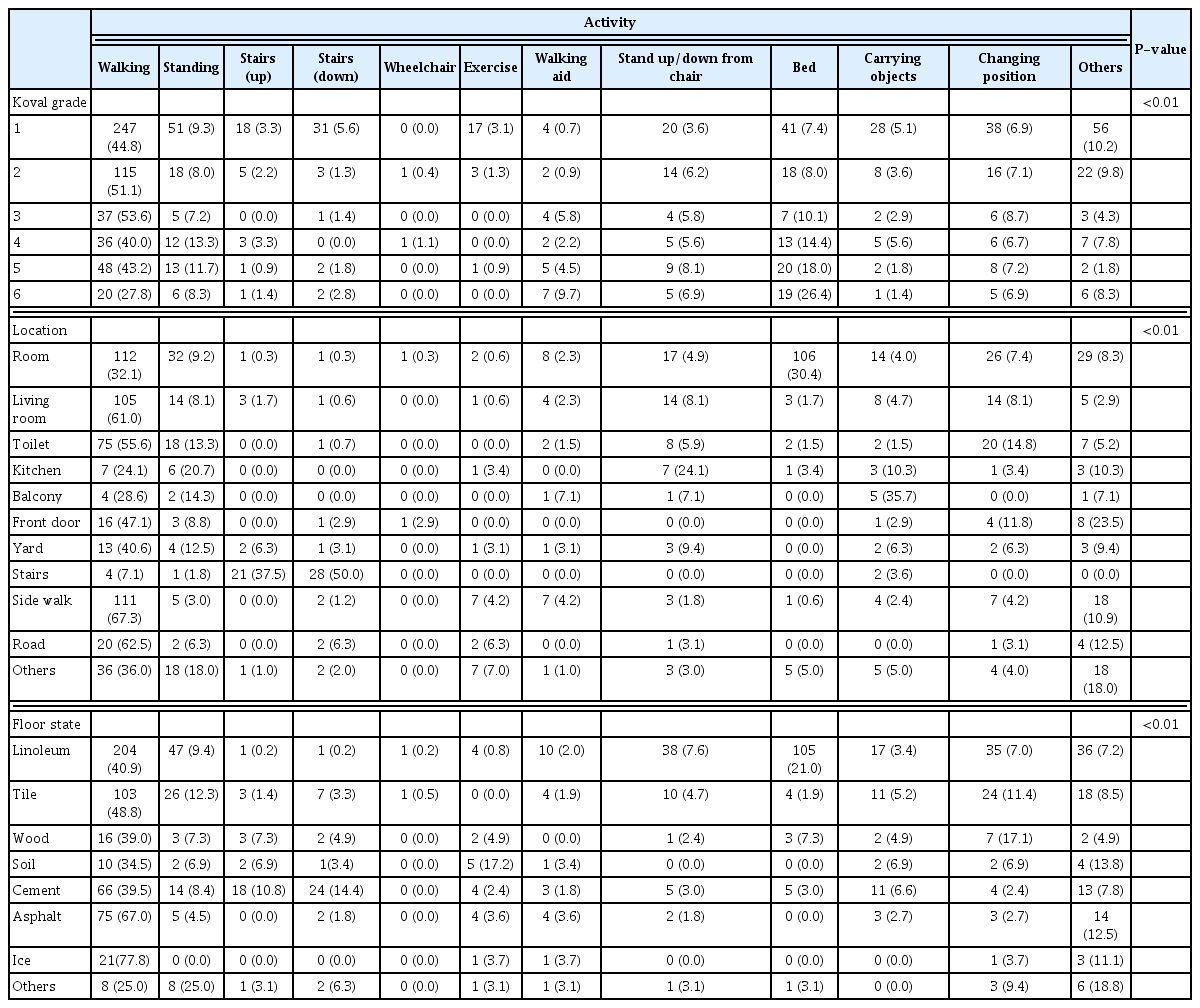
Comparing between sexes, male patients were younger (P<0.01) with a low osteoporosis treatment rate (9.0% treatment rate vs. 25.4% in females; P<0.01), and better ambulatory function (Koval 1, 57.3% vs. 46.6%; P<0.05). Voiding state showed a difference, in which dysuria was higher in male patients and urgency and incontinence were higher in female patients (P<0.01) (Table 1). About a place of fall, proportion of outdoor fall was higher in males (39.8% vs. 28.8% in females; P<0.01) but indoor fall was more frequent in both sexes. Room was the most common location of fall in both groups, and room, living room, toilet and sidewalk consisted of over 70% of fall locations, but male patients showed a higher proportion for sidewalk (21.9 vs. 12.4% in females; P<0.01). Linoleum was the most common condition of floor in both sexes, but male patients showed higher proportion of asphalt and ice (15.1% and 4.3% vs. 8.3% and 1.8% for females; P<0.01). In both sexes, walking was the most common activity during falls, and slippage was the most common perceived reason for falls (Table 2). When activity is correlated with Koval grade, location, and floor state, walking was the most prevalent activity through all 3 variables (P<0.01). With increasing Koval grade, walking decreased, and bed-related falls increased (P<0.01). Regarding the location of room, bed-related fall was as frequent as walking (P<0.01). Regarding floor state for ice, 77.8% of falls occurred during walking (Table 3).
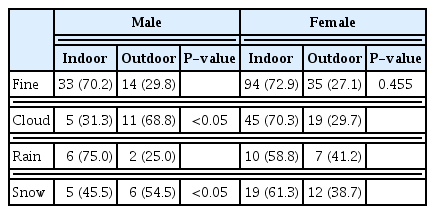
Comparing between seasons, proportion of osteoporosis treatment was lowest in winter in both sexes (2.4% for males, 19.9 for females; P=0.109 & P<0.05 male and female), posterior fall highest in summer in females (42.9%; P<0.01). There was no difference in the mean number of fractures, diagnosis, voiding problem and Koval stage according to seasons in both sexes (Table 4). When fall related extrinsic factors were compared weather, time, place, location, activity during fall showed no difference according to seasons in both sexes. About floor condition, linoleum, and ice were highest in winter (P<0.01) and slippage was more common in the winter season (P=0.194 and P< 0.01 for male and female) (Table 5). Results of sub-analysis in the winter season between the place of fall and weather showed no difference in proportion place according to weather in female patients, but male patients showed a higher proportion of fall in cloudy and snowy days outdoors (P< 0.05) (Table 6).
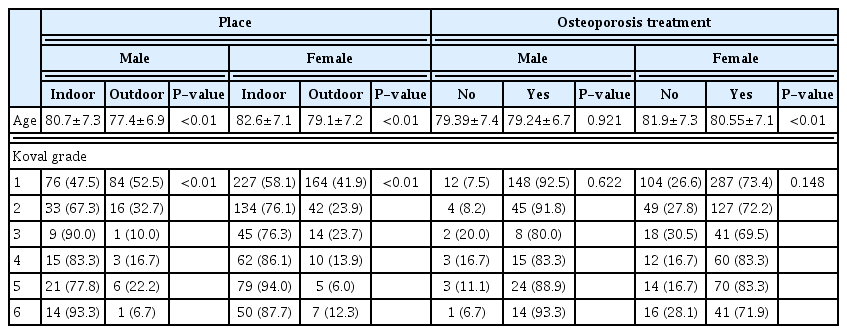
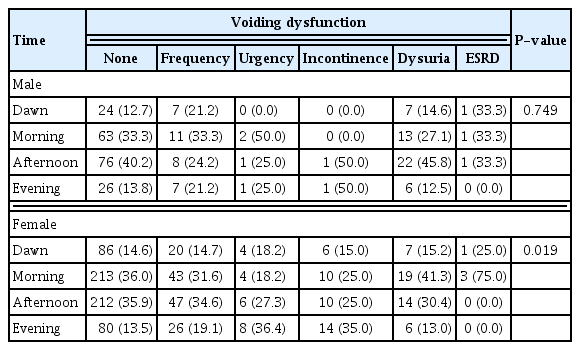
When Age and Koval grade was compared with place and osteoporosis treatment, indoor fall patients were older than outdoor fall patients in both sexes (P<0.01) and with increasing Koval grade, indoor fall increased (P<0.01). About osteoporosis treatment, age of male patients showed no difference in osteoporosis treatment, but in female patients, osteoporosis treatment group was younger compared to non-treatment group. (P<0.01) There was no difference in osteoporosis treatment rate according to Koval grade (Table 7). When voiding status was compared with time of fall, male patients showed no difference but female patients with urgency and incontinence showed higher number of falls during evening (Table 8).
DISCUSSION
Fall prevention is an important strategy for reducing hip fracture. However, sexual and seasonal variation of intrinsic and extrinsic factors related to hip fracture including Koval stage and voiding dysfunction has not been investigated yet. The aim of this study was to find the relationship between hip fracture-related variables according to season and sex.
In both sexes and throughout all seasons, indoor fall was prevalent and there was no difference in proportion between 2 groups including winter season. This is in accordance with previous studies, which showed indoor fall injuries higher irrespective of the season.[12–14] This can be explained by the previous study reporting snowy conditions forcing frailer elderly people to stay indoors.[15] Moreover, our study showed increasing Koval grade was associated with increasing indoor fracture in both sexes which is in accordance with previous studies.[16–18] The importance of this phenomenon is that indoor fractures are 3 times more likely to result in future mobility limitations [19] and are associated with higher mortality,[16] which necessitates more indoor prevention strategies needed for the prevention of this population. One more thing to consider is that compared to the study by Kim et al.[20] which reported among elderly falls, floor/ground state was highest for cement/asphalt and soil (outdoor), in contrast to our study (linoleum highest, which is indoor). This may imply indoor falls have a higher probability resulting in hip fracture. Therefore, in old frail patients, indoor fall prevention programs should be more rigorously emphasized for the prevention of hip fractures, even in the winter season.
The result of this study showed a higher proportion of outdoor fall in male patients. This may be explained by younger age, which is in accordance with a previous study,[13] and better ambulatory function in male patients as shown in this study. This is in accordance with previous study that outdoor fallers were more likely to be male and younger and have higher physical functioning.[21,22] In another point of view, this can also be explained by the higher outdoor time spent outdoor in male patients [21] resulting in different fall locations. Moreover, considering the difference between mean age and Koval stage between indoor and outdoor fall groups of both sexes, the influence of fall location on age and ambulatory function is becoming evident. Additionally, in subgroup analysis for the winter season, male patients showed higher outdoor fall in cloudy and snowy weather, in contrast to female patients showing consistent indoor dominance regardless of weather, which was not reported until now. Thus, especially for male patients, outdoor fall prevention should be more emphasized. This can also have another important implication because numerous international and national health agencies are encouraging active living and recommend outdoor exercise for the prevention of osteoporosis.[23,24]
Regarding activity during fall, walking was the most prevalent in both sexes and throughout all seasons. This is in accordance with previous studies.[17,21,25,26] Moreover, this phenomenon was observed for all Koval stages and all floor states (P<0.01). This may be the reason why exercise including balance and functional exercise are effective for reducing the rate of falls and fall-related outcomes [8,27] rather than multifactorial interventions. Therefore, safe walking education, including refraining from ice, should be emphasized for all patients.
One more interesting finding that needs to be mentioned is that among the cases in which falls occurred in room, transfer from/to bed was as common as walking. Additionally, with increasing Koval grade, the proportion of fall related to bed increased. This may have clinical importance as along with walking exercise education, education on precautions when transferring from bed can have a high possibility of reducing hip fracture especially in frail patients. Moreover, as about 30% of compression fractures of the spine is known to occur while in bed, training of transfer from/to bed and motion during bed can have additional effect for the prevention of hip and spine fragility fractures, which both is known to be associated with is increased morbidity and mortality.
Most fractures occurred in the morning and evening. This is in accordance with previous studies that showed a majority of falls among home-dwelling elderly persons commonly take place during the period of maximal activity [28, 29] and this can be explained by our data that most patients were walking at the time of fracture. However, when voiding function is considered, female patients showed a higher proportion at night time in urgency/incontinence group. The association of urgency/incontinence with a higher risk of falls has been reported in several studies.[30,31] However, increased nighttime fall risk resulting in hip fracture has not been reported until now. This can be explained by increased nocturnal voiding, and may be because of rushing to the bathroom in a dark situation to avoid incontinent episodes. Thus, identification and treatment of urgency/incontinence, including bladder training, timed or prompt voiding, and environmental modifications (e.g., a bedside commode),[32] may be an effective intervention for reducing the risk of falls, especially at night time.
Although osteoporosis treatment rate was lower in male patients, the rate itself was also low in female patients. Mean age showed no difference according to osteoporosis treatment in male patients, but in female patients, treatment group was younger than the no-treatment group. This is in contrast to the increasing prevalence of osteoporosis with age,[33] which should show higher age in osteoporosis treatment group, and this result is important as increased age itself is a risk factor of functional loss after hip fracture.[3] Therefore, more rigorous effort should be applied for the diagnosis and treatment of osteoporosis with increasing age. Moreover, our result shows no association of osteoporosis treatment with Koval grade in both sexes. This finding is important as probability of falls is known to be increased in poor ambulatory status [34] and considering more indoor fractures in high Koval stage and indoor fracture resulting in more disability,[19] treatment targeted for these population should be seriously considered as an public health issue.
One more finding that needs to be mentioned is that in the winter season, the proportion of osteoporosis non-treated group was higher than treatment group. This may be explained by vitamin D issues,[35,36] which can result in decreased muscle strength and coordination [37] increasing risk of falls, as Seoul is a northern region with cold winters and subzero temperatures with ultraviolet-B deficiency in winter.[38] More studies are needed to reveal this association but osteoporosis treatment may become a more powerful method for preventing hip fractures especially in winter. This issue is more important as winter epidemics of fracture are known to overwhelm medical resources.[39,40] including increased length of stay,[41,42] and wintertime hip fracture surgery is associated with an increased risk of mortality [43] and revision procedures.[44]
There are some limitations of our study. We were unable to determine the potential effect of temperature in our subject sample. However, considering the same proportion of indoor/outdoor falls in both sexes throughout all seasons, this variable may have minimal effect on the fall risk resulting in fracture. Second, our study was a tertiary hospital single institution study which cannot represent Korea’s national data. However, we tried to make minimal bias by collecting 9-year data on a raw. Third, we did not see the effect of underlying disease. However, we tried to evaluate the risk and pattern of fracture according to Koval classification, which is directly related to ambulatory function and level of activity. Fourth, we used a questionnaire for this study which is prone to make mistakes in reporting due to memory issues. However, we tried to minimize this possibility by having an interview before discharge of the patient (usually within 2 weeks) and dedicating the interviewer to junior resident.
In conclusion, to reduce hip fracture incidence, strategies for indoor fall prevention and vigilant osteoporosis diagnosis and treatment should be considered important all through the seasons especially for frail elderly patients. For male patients, outdoor fall prevention should be more considered, and in female patients with voiding dysfunction, education for nighttime falls should be provided.
Notes
Ethics approval and consent to participate
The study was conducted in accordance with the principles of the ethical guidelines of the 1975 Declaration of Helsinki.
Conflict of interest
No potential conflict of interest relevant to this article was reported.