INTRODUCTION
Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture.[
1] Measurement of bone mineral density (BMD) is a central component in the diagnosis of osteoporosis. Dual energy X-ray absorptiometry (DXA) measurement of BMD is considered the gold standard in diagnosing osteoporosis and assessment for the risk of osteoporotic fracture.[
2]
Recently, spine-hip discordance (SHD) is increasingly investigated by researchers. By the definition of the World Health Organization (WHO),[
3] minor discordance is osteopenia at 1 site and normal or osteoporotic BMD at another, and major discordance is the normal bone density at 1 site and osteoporosis at another.[
4] Other definition also exists, which uses a difference in T-score of least 1 standard deviation (SD; regardless of any change in diagnostic class) as minor discordance [
5] or T-score difference of 1.5 SD as a discordance.[
6] These discordances are known to be associated with risk of fracture.[
7,
8]
However, the prevalence of SHD and its clinical implications were not assessed. Considering the growing interest in SHD and the importance of hip fracture, which results in high mortality, loss of independence, lower quality of life, and high rate of socioeconomic burden,[
9] the clinical implication of SHD in hip fracture patient needs investigation. The purpose of this study is to assess the prevalence and clinical implication of SHD and investigate the cause of SHD in elderly patients with hip fractures.
METHODS
1. Study population
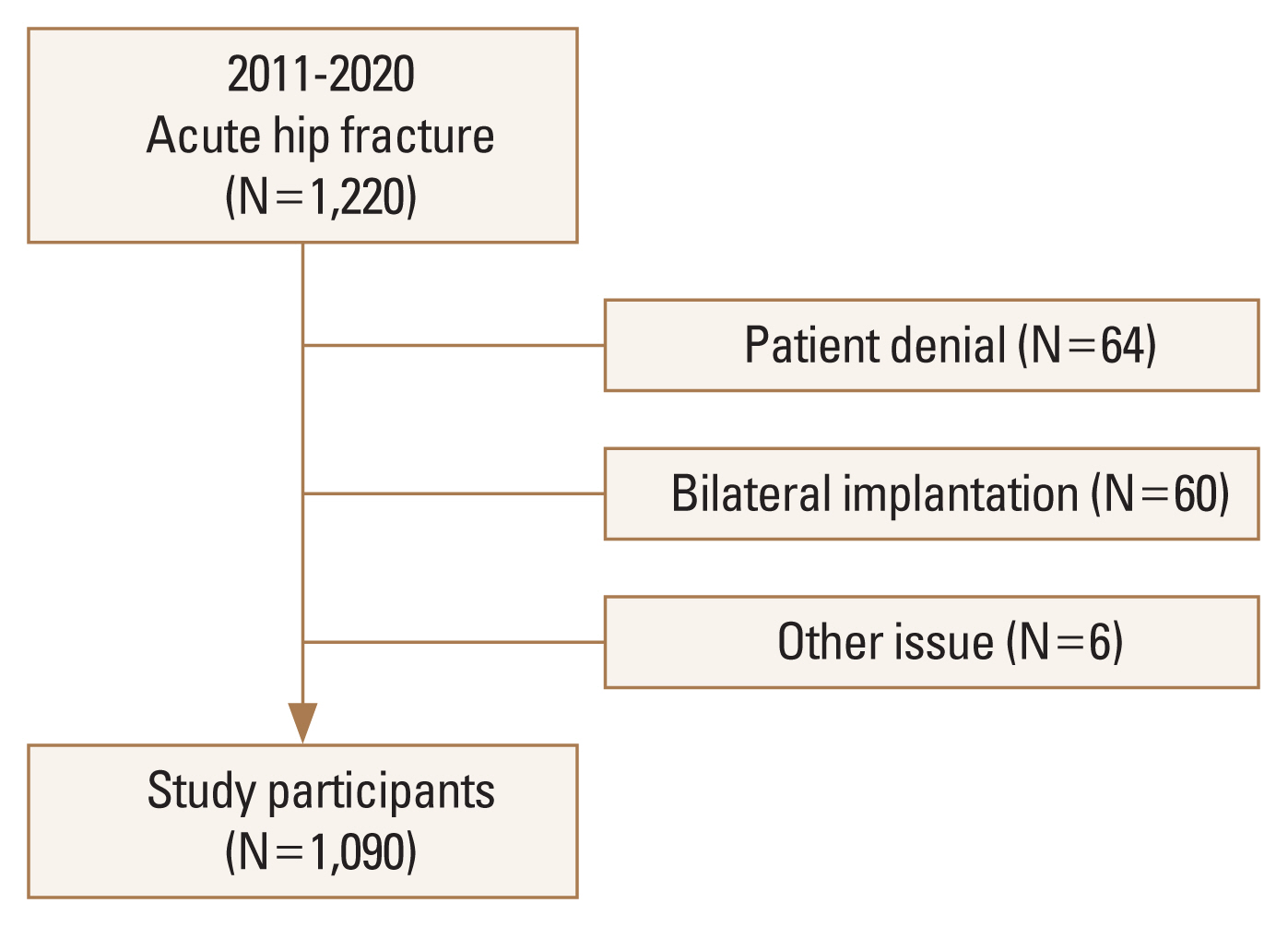
Between 2011 and 2020, patients aged >65 years who were admitted for surgery due to acute hip fracture were eligible for this study. During this period, 1,220 patients visited our emergency department due to a fresh hip fracture. Of these patients, 64 patients could not undergo DXA due to patient refusal, 60 excluded due to bilateral implantation state, and 6 for other issue. As a result, data on 1,090 patients were analyzed for this study (
Fig. 1).
2. Bone density measurement
The areal BMD (aBMD) of the lumbar spine (LS) was acquired using DXA scan images (Lunar Prodigy Advance; GE Lunar, Madison, WI, USA). Daily calibration and quality assurance testing were performed, and the coefficient of variation for precision in measuring the aBMD of the LS was 0.34%. The aBMD was expressed in g/cm
2, and the T-score was defined as the number of SDs from the mean aBMD for a reference group from the general South Korean population. The diagnosis was made according to the WHO classification using T-scores as follows. T-scores −2.5 SDs were defined as osteoporosis, T-scores between −2.5 and −1.0 SDs were defined as osteopenia, and T-scores >1.0 SD were defined as normal. The difference in the discordance between L1-4 and femur neck BMD was defined as ≥1.5 SD, and was divided into 3 groups: LS low (LL) discordance, no discordance (ND) and femur neck low (FL) discordance groups.[
6]
3. Data collection
Since 2011, data including age, sex, height, weight, American Society of Anesthesiologists (ASA) score, BMD of L1-4, femur neck were prospectively collected. And for this specific study, data were retrospectively reviewed from November 2021 to January 2022 compared with the original data on the electrical medical record system. After surgery, patients were followed up at our outpatient clinic at 6 weeks, 6 months, 1-year, and yearly thereafter. Patients who were lost to follow-up within 1 year after operation were contacted by phone to check for mortality. Also for missing cases, mortality was checked with medical records or the expiration of the social security number.
4. Cause of discordance
To evaluate the cause of discordance, L-S spine anteroposterior/lateral radiographs of discordant cases were reviewed. The cause of discordance was classified into physiologic, pathophysiologic, and artifacts according to the description by Woodson [
3]. Cases were classified as physiologic cases when there was no pathologic or artifacts lesion. Cases were classified as pathophysiologic when there was vertebral osteophytosis, endplate and facet sclerosis, ankylosing spondylitis, osteochondritis, compression fracture, or aorta calcification. Cases with bone cement, implantation, and metal particles were classified as artifact groups. The X-ray was reviewed by 2 experienced orthopedic surgeons, and the most contributing abnormality was decided by discussion between the 2 and classified accordingly.
5. Statistical analysis
All measurements were reported as the mean±SD. For comparison, ANOVA was used for continuous variables and post hoc analysis was done with least significant difference. A χ2 test was used for categorical variables. SPSS for Windows statistical package (version 27.0; SPSS Inc., Chicago, IL, USA) was used, and a P-value of less than 0.05 was considered significant.
RESULTS
Of the 1,090 patients, 271 (24.9%) were male and 819 (75.1%) were female. The diagnosis was 453 femur neck fractures (41.6%), 600 intertrochanteric fractures (55.0%), and 37 subtrochanteric fractures (3.4%). ASA was one in 18 cases (1.7%), 2 in 445 cases (40.8%), 3 in 617 cases (56.6%), and 4 in 10 cases (0.9%). The 769 cases were diagnosed with osteoporosis (70.6%), and 1-year mortality rate was 10.8%. Discordance was observed in 504 cases (46.2%). Baseline demographic information and patient characteristics are summarized in
Table 1.
Compared with sex differences, although height and weight were higher in male (
P<0.01), body mass index (BMI) was higher in female (
P<0.05). BMD of L1-4 and neck was higher in male and 1-year mortality was higher in male (
P<0.01). ND was lower and FL was higher in male group, and the prevalence of osteoporosis was higher in female group. Overall, between sexes, age, height, weight, BMI, L1-4 BMD, femur neck BMD, 6-month mortality, 1-year mortality, discordance, osteoporosis showed a difference (
Table 1).
Compared with 3 different groups in males regarding clinical implications such as diagnosis, ASA, and mortality, FL group was older than ND group and showed higher body weight and BMI compared to LL and ND group (
P<0.05). LS BMD was different between groups (
P<0.01). There was no difference in mortality between groups (
Table 2).
Comparing with 3 different groups in females regarding clinical implications such as Diagnosis, ASA, and mortality, FL group showed higher body weight and BMI compared to LL and ND group (
P<0.01). LS T-score was different between all groups, but femur neck T-score was higher in LL group compared to ND and FL group (
P<0.01) There was no difference in mortality between groups (
Table 3).
The cause of discordance was different between groups. In both sexes, physiologic discordance was dominant in LL group and pathologic discordance was dominant in FL group (
P<0.001) (
Table 4).
DISCUSSION
SHD is known to increase fracture risk. However its prevalence and clinical implication have not been investigated in hip fracture patients. The purpose of this study was to determine the prevalence and association with mortality in SHD group compared to ND group and investigate the cause of SHD in hip fracture patients. The results of this study was shown that pattern of discordance in each sex (ND>FL>LL) and in both sexes, and FL was associated with higher body weight and BMI. The most common causes of discordance in both sexes were physiologic in LL group, and pathophysiologic in FL group, respectively. However, discordance was not related to 6 months and 1-year mortality in both sexes.
The prevalence of discordance shown in this study was higher than those of the previous study,[
6] Hong et al. [
6] assessed the prevalence and characteristics of individuals with BMD discordance using a total of 3,233 men aged ≥50 years and 2,915 postmenopausal women. They defined T ≥1.5 as a standard for spine hip BMD discordance and found 417 men (12.9%) and 290 women (10%) exhibited spine-femur BMD discordance. Of them, LL and FL in males and females were 152 (4.7%) vs. 159 (5.5%) and 265 (8.2%) vs. 131(4.5%), respectively. In this study, prevalence of LL and FL in males and females were 12 (4.4%) vs. 32 (4.0%) and 79 (29.2%) vs. 164 (20.0%), respectively. The difference in prevalence of discordance might be related to differences in demographic characteristics in 2 studies. Additionally, our group was older than the previous study, which also can explain a higher proportion of discordance in our study.[
10-
12]
Moreover, population group in this study was elderly patients with fragility hip fracture. The risk factor of hip fractures was known to be old age, osteoporosis, visual impairment etc. [
13] and femoral neck BMD is also known as a risk factor of hip fracture.[
14] Recently discordance has been proposed as a risk factor for fracture.[
7,
8] However, as shown in this study, not the discordance itself, but the FL type of discordance may be a strong risk factor for femur fracture which needs further investigation.
In this study, body weight and BMI in FL group were higher than those of LL and ND group in both sexes. This is in accordance with the previous study.[
6] Moreover, what should be emphasized, this finding is in accordance even with lower BMI values in our study group. Previously, BMD of femoral neck is known to be associated with type 2 diabetes mellitus and metabolic abnormalities [
15,
16] which may explain the association between BMD and FL group. However, our study shows major determinant to decide the type of discordance is L1-4 BMD (
P<0.01), not the femur neck value. This discrepancy might be related to the difference in patient characteristics.
Discordance in both sexes was not associated with 6 months and 1-year mortality. The pattern between ND and LL/FL was different. In ND group 1-year mortality was about twice compared to 6-month mortality. However, LL/FL group showed no or minimal change in mortality between the 2 time periods. Although further follow-up study is necessary to access clinical implications between mortality and type of discordance, this study could not confirm a significant relationship between mortality and discordances.
The cause of discordance was different between groups. In both sexes, physiologic discordance was dominant in LL group and pathologic discordance was dominant in FL group. However, what is more important, there were also pathological findings in LL group and also physiologic findings in FL group. This implies that the true degree of discordance can be underestimated or overestimated in both groups due to their pathology. Therefore, discordance should be assessed with caution. Additionally, as FL group was associated with a high proportion of pathology (75.9% and 78.0% each), the effect of BMI, which is described previously, can be considered to affect the pathologic process of the spine resulting in high spine BMD.
This study has several limitations. First, this study was retrospectively designed and selection bias was inevitable. Second, patients visiting tertiary referral center can have different profiles compared to whole hip fracture population. However, in Korea, hip fractures are mostly treated in tertiary center, and the sample size of our study can make the generalization of our result more acceptable. Third, association underlying implication of FL could not be revealed in this study. Further study might be necessary to confirm implication of FL in hip fracture population.
In conclusion, hip fracture patient groups showed lower ND and higher FL compared to the general population. True discordance should be judged carefully for pathologic and artifact reasons. The clinical implication of SHD needs more verification.












 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



