Vitamin D Status and Response to Initial Vitamin D Supplementation in Korean Women with Osteoporosis
Article information
Abstract
Background
The aim of this study is to evaluate whether the optimal vitamin D level is achieved after taking recommended dose in vitamin D deficient patients.
Methods
This was a retrospective study. Women (n=52) first diagnosed with osteoporosis were recruited in outpatient clinic. They were recommended to be exposed to sun light for more than 30 min a day. Subjects were divided into 3 groups according to serum 25-hydroxy-vitamin D3 (25-[OH]D3) status: deficiency (less than 20 ng/mL), insufficiency (20-30 ng/mL) and sufficiency (30 ng/mL or more). Insufficient and sufficient patients received the recommended dose (1,000 IU/day) but deficient patients received recommended or double dose (1,800-2,000 IU/day). We compared 25-(OH)D levels at baseline and after vitamin D supplementation for 3 months.
Results
Median (interquartile range) serum 25-(OH)D concentration at baseline was 15.10 (13.30-16.97) ng/mL and the proportion of deficient, insufficient and sufficient groups were 69.2%, 23.1%, and 7.7% respectively. The optimal 25-(OH)D level (30 ng/mL or more) was achieved in 83.3% of insufficient patients with the recommended dose and was did in 55.6% of deficient patients with recommended dose (P=0.117). However, 88.9% of the deficient patient with double dose achieved optimal level (P=0.030).
Conclusions
About 44% of vitamin D deficient patients did not attain the optimal level of serum 25-(OH)D despite recommended daily intake of vitamin D to 1,000 IU in patients with osteoporosis. Follow-up of serum 25-(OH)D levels may be required for vitamin D supplementation in vitamin D deficient patients with osteoporosis.
INTRODUCTION
Vitamin D deficiency is related with parathyroid hormone-induced bone resorption and changes in calcium homeostasis, and most studies have addressed that the increase in serum vitamin D levels reduces the risk of fracture.[1]
Vitamin D promotes the absorption of calcium and phosphorus in the small intestine. In a vitamin D deficient state, the intestine typically absorbs 10-15% of dietary calcium, but in a vitamin D sufficient state, 30-40% is absorbed from the diet.[2] A long-term severe state of vitamin D deficiency lowers the efficiency of calcium and phosphorus, and induces osteomalacia by impairing mineralization in the synthesis of new bone matrix.[3] Vitamin D deficiency with a less severe clinical state may lead to bone mineral density (BMD) decrease in the lumbar spine and hip by increasing bone metabolism rate induced by a rise of serum parathyroid hormone due to declined intestinal calcium absorption.[1,4,5]
The American National Osteoporosis Foundation recommends an intake of 800-1,000 IU of vitamin D per day, and the Korean Society for Bone and Mineral Research also recommends a vitamin D intake of at least 800 IU/day.[6] Adequate serum vitamin D level for fracture prevention is known to be 25-hydroxy-vitamin D3 (25-[OH]D3) at or above 30 ng/mL (75 nmol/L).[7] Of all Korean adult women, 6.4% have a 25-(OH)D level at 30 ng/mL (75 nmol/L) or higher (adequate level), while 49.9% have a 25-(OH)D level of less than 20 ng/mL (deficiency level), accounting for a large percentage of the population.[8] Despite the recommended intake of vitamin D (800-1,000 IU/day), Korean women with a high prevalence of vitamin D deficiency did not reach adequate 25-(OH)D levels.
This study was performed to evaluate the degree of reaching the optimal vitamin D level according to vitamin D intake amount (recommended or high-dose) in 3 groups divided according to 25-(OH)D levels (sufficiency, insufficiency, deficiency). Subjects were vitamin D deficient patients diagnosed with osteoporosis and receiving vitamin D supplements for the first time.
METHODS
1. Subjects and research period
This study retrospectively analyzed female patients first diagnosed with osteoporosis in the Department of Family Medicine at a University Hospital from March 2011 to February 2013. The 25-(OH)D test was conducted before considering supplementation with vitamin D in those patients, and they were recommended to be exposed to sunlight for more than 30 min a day. Follow-up was done 3 months after vitamin D supplementation. Among a total of 72 patients first diagnosed with osteoporosis, 52 patients were included in the study, excluding 18 women who did not underwent the 25-(OH)D test twice and 2 women who consumed more than 2,000 IU/day of vitamin D. All subjects were living in the central region at 30 degrees north latitude in Korea.
The occupations of the subjects were identified as 9 types recorded in the inquiry form. Patients exercising for more than twice a week (a total of more than 60 min/week) were classified as exercise group and those not exercising as non-exercise group.
2. Measurement of vitamin D3 concentration
Vitamin D3 concentration was measured with serum 25-(OH)D levels at baseline and after vitamin D supplementation for 3 months. Vitamin D status was assessed using radioimmunoassay (Dream Gamma-10, Belgium). The functional sensitivity of the assay was 4.01 ng/dL (coefficient of variation of 18.5%).
Most previous studies defined vitamin D insufficiency as serum 25-(OH)D below 20 ng/mL. Serum 25-(OH)D levels over 30 ng/mL suppress serum parathyroid hormone and reduce fracture risk.[1,6,9] Bases on these findings, subjects were divided into 3 groups according to serum 25-(OH)D status: deficiency (20 ng/mL or below), insufficiency (20-30 ng/mL) and sufficiency (30 ng/mL or over).
3. Vitamin D dose
All patients consumed 1,000 IU/day of vitamin D (cholecalciferol), in combination with 500 mg/day calcium. Patients taking only the recommended dose were divided into recommended dose group (cholecalciferol 1,000 IU/day). Deficient patients with less than 20 ng/mL of serum 25-(OH)D received 1,000 IU/day of cholecalciferol in addition to the daily recommended dose and classified as high dose group. Among high dose patients, taking alendronate-cholecalciferol (alendronate 70 mg+cholecalciferol 5,600 IU) per week was considered the same as taking 1,800 IU/day of cholecalciferol. Patients receiving the other osteoporosis medication were given 2,000 IU/day of cholecalciferol. Subjects were prescribed with Fosamax Plus D (MSD) as alendronate-cholecalciferol and Dicamax 1000 (Dalim Biotech, Seoul, Korea) as cholecalciferol.
4. Statistical analysis
Serum 25-(OH)D levels were represented as median values (interquartile range), since the data were not normally distributed. Differences (in variables) between groups were analyzed with the Mann-Whitney U test for comparison of vitamin D levels between exercise and non-exercise groups. Serum 25-(OH)D levels at baseline and after vitamin D supplementation were analyzed using the Wilcoxon signed-rank test. Of all patients in deficient and insufficient groups, the percentage of patients who reached sufficient status after taking the recommended dose of vitamin D was analyzed with the Fisher's exact test. The percentage of deficient patients who reached sufficient status after receiving the recommended dose or high dose of vitamin D was analyzed with the same method. All statistical data analyses were performed using IBM SPSS Statistics version 21 (SPSS Inc., Chicago, IL, USA). P-values of less than 0.05 were considered statistically significant.
RESULTS
1. General characteristics of subjects and 25-(OH)D concentration
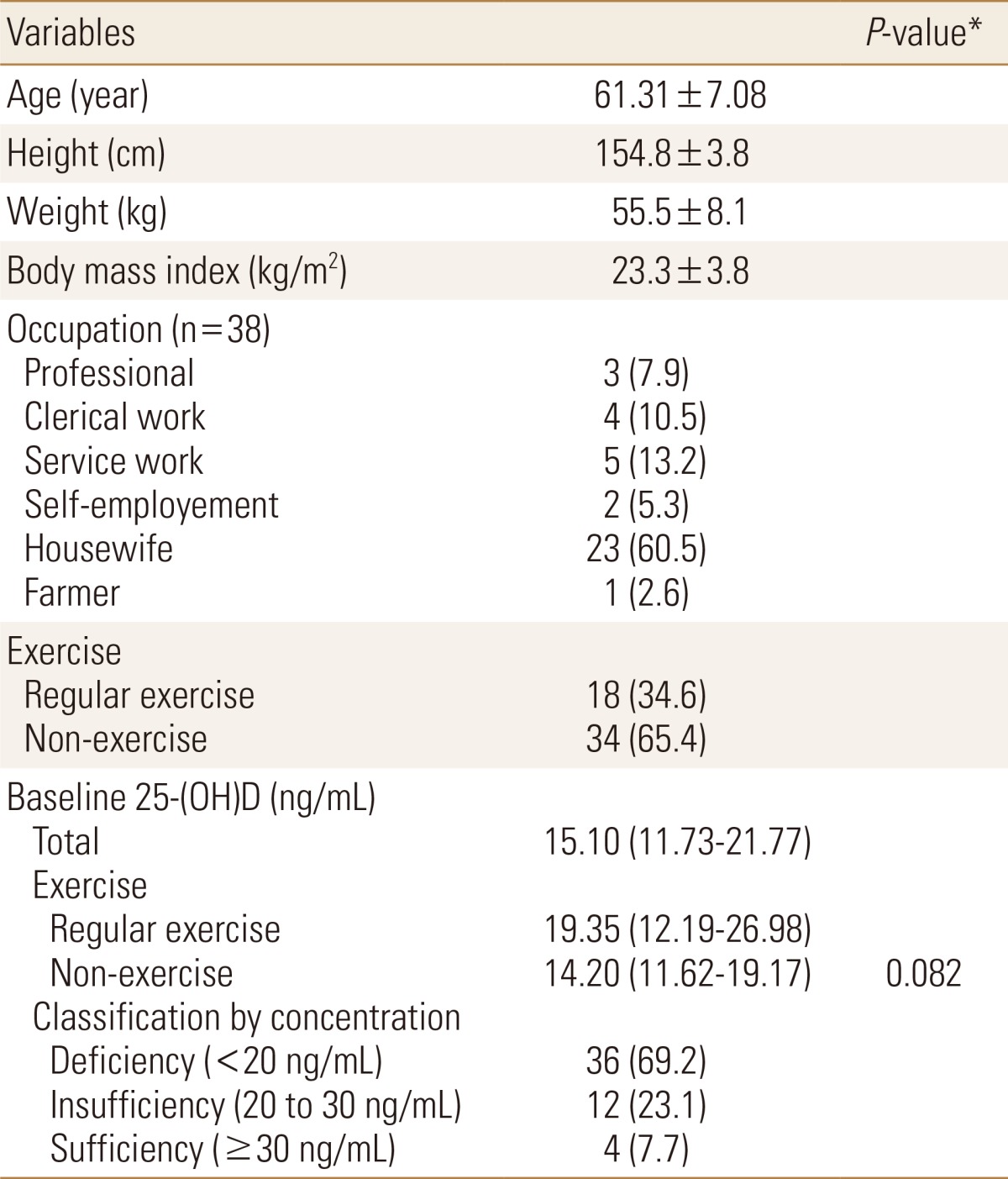
The mean age of 52 subjects was 61.31±7.08 (50-84). The mean height and weight were 154.8±3.8 cm and 55.5±8.1 kg, respectively. The average body mass index (BMI) was 23.3±3.8 kg/m2. Occupation was identified in 38 out of 52 subjects. Housewife accounted for the largest proportion of all occupations at 60.5%, followed by service work (13.2%), clerical work (10.5%), professional (7.9%), self-employment (5.3%), and farmer (2.6%).
Median (interquartile range) serum 25-(OH)D concentration at baseline was 15.10 (11.73-21.77) ng/mL. Serum 25-(OH)D levels were 19.35 (12.19-26.98) and 14.20 (11.62-19.17) ng/mL in exercise and non-exercise groups, respectively, showing no significant difference (P=0.082). Of 52 subjects, 36 (69.2%) belonged to the vitamin D deficient group, 12 (23.1%) to insufficient group, and 4 (7.7%) to sufficient group (Table 1).
2. Increase in 25-(OH)D concentration after vitamin D intake
Changes in the increase of serum 25-(OH)D levels before and after vitamin D intake are shown in Table 2. After taking 1,000 IU/day (recommended dose) of vitamin D supplements, the median (interquartile range) serum 25-(OH)D levels increased significantly from 15.10 (13.30-16.97) to 30.27 (26.63-38.14) ng/mL (P<0.001) in vitamin D deficient group and from 23.66 (21.21-26.08) to 41.73 (30.40-55.96) ng/mL (P=0.003) in insufficient group. On the contrary, there was no significant increase in vitamin D sufficient group. After taking 1,800-2,000 IU/day (high dose) of vitamin D, the median (interquartile range) serum 25-(OH)D level showed a significant increase from 11.50 (9.86-12.49) to 42.47 (38.11-52.15) ng/mL (P<0.001).
3. Rate of reaching optimal levels after vitamin D intake
Table 3 shows the rate of reaching optimal serum 25-(OH)D levels (30 ng/mL or above) in insufficient group (30 ng/mL or below) after vitamin D supplementation. The rate of achieving target serum 25-(OH)D levels was 55.6% in deficient group and 83.3% in insufficient group after taking 1,000 IU/day of vitamin D supplements, showing no significant difference (P=0.117). In deficient group, the rate of reaching adequate levels was significantly higher in patients taking 1,800-2,000 IU/day than in patients taking 1,000 IU/day of vitamin D (P=0.030).
DISCUSSION
This study compared response to initial vitamin D supplementation according to doses (800-1,000 IU/day or 2,000 IU/day) of vitamin D supplements in patients first diagnosed with osteoporosis by dividing them into 3 groups according to serum 25-(OH)D concentration (deficiency, insufficiency and sufficiency). Despite plenty of data on vitamin D deficiency in Korean women, data on required vitamin D amount addition to the recommended dose in actual clinical situations are rarely found.
In a study on 5,847 Korean adults, 6.4% of women had adequate serum 25-(OH)D levels of more than 30 ng/mL, while 67.4% had deficient levels of less than 20 ng/mL.[7] Comparable to the results of our study, 8% had optimal 25-(OH)D levels, while 69.0% were deficient status among patients first diagnosed with osteoporosis. Although this study had a small sample size of 52, the distribution of vitamin D concentrations was comparable to that of previous studies comprising larger sample sizes. There was no significant difference in serum 25-(OH)D levels between exercise and non-exercise groups. Even though it is difficult to explain these facts with the findings of this study, this is anticipated to be attributable to no difference in sunlight exposure time and area between exercise and non-exercise groups.
To raise a serum vitamin D level of 10 ng/mL, daily vitamin D intake to 1,000 IU is typically required for 3-4 months.[10] According to the results, patients taking 1,000 IU/day of vitamin D supplements in deficient and insufficient groups, 25-(OH)D level was increased by about 17 ng/mL, approximately 7 ng/mL higher than the estimated level. In a previous study (December to March) on patients with diabetes, 25-(OH)D concentration was higher than that of control group by 14.6 ng/mL after administration of daily dose of 1,000 IU cholecalciferol for 24 weeks.[11] A smaller increase in 25-(OH)D level is assumed to be resulted from research period, excluding summer season, in the previous study performed from December to March, unlike our study period. However, in another previous study (November to January) on Koreans, 25-(OH)D level was higher than that of control group by 17.0 ng/mL (equivalent to 8.5 ng/mL in 1,000 IU) after administration of 2,000 IU cholecalciferol daily.[12] These contradicting results were attributed to the fact that various factors (seasonal differences in the amount of daylight, sunlight exposure time and area and etc.) other than vitamin D, potentially increasing 25-(OH)D concentration were not accurately reflected in results. In deficient patients taking 1,800-2,000 IU/day of vitamin D supplements, 25-(OH)D concentration was raised by about 32 ng/mL, 12 ng/mL higher than the estimated value of 20 ng/mL. Since the authors did not evaluated sunlight exposure time and area, we were unable to determine whether the higher increase of 25-(OH)D levels in high dose group than recommended dose group was caused by vitamin D deficiency or differences in sunlight exposure.
Among deficient patients in this investigation, 55.6% maintained optimal 25-(OH)D levels of greater than 30 ng/mL after daily vitamin D intake to 1,000 IU, while 88.9% maintained optimal levels after daily vitamin D intake to 1,800-2,000 IU. In a previous study on Spanish women after vitamin D administration for 3 months, women maintaining serum 25-(OH)D levels of more than 30 ng/mL were 27.7% in the group with vitamin D intake of 800-1,000 IU/day, 53.6% in the group with 1,000-1,600 IU/day, and 90.2% in the group with 1,600 IU or over.[13] In another study on white American women, the Recommended Dietary Allowance (RDA) was obtained as daily reference values for reaching target serum 25-(OH)D levels in more than 97.5% of women. The RDA values were 800 IU/day at 20 ng/mL and 1,600 IU/day at 30 ng/mL as standard.[14]
Postmenopausal women have a higher risk of falling or fracture when they do not maintain serum 25-(OH)D levels higher than 30 ng/mL. It is crucial to sustain adequate 25-(OH)D levels. According to the results, about 69% of osteoporosis women had vitamin D deficiency (less than 20 ng/mL) and about 44% failed to reach above the optimal level of 30 ng/mL despite recommended daily vitamin D intake to 1,000 IU. On the other hand, most deficient patients (88.9%) were able to maintain adequate levels after administration of high-dose (1,800-2,000 IU/day) vitamin D. Since the authors did not consider all influential factors on vitamin D concentration, we were unable to conclude that high-dose vitamin D supplementation is required in vitamin D deficient group. However, follow-up of 25-(OH)D levels for determining increases in the daily recommended dose of vitamin D in deficient patients may be beneficial in maintaining optimal levels of 25-(OH)D.
The limitations of the present study are as follows: First, a limitation of this retrospective study is that the experimental (high-dose vitamin D supplementation) and control (recommended-dose vitamin D supplementation) groups were not discriminated. Thus, the study results are limited in actual clinical application. Second, subjects are not representative of the Korean population by involving patients from a single university hospital. Third, the study is limited by the relatively small sample size. Nevertheless, this study was significant in that it analyzed response to initial vitamin D supplementation and the percentage of patients who did not reach optimal serum 25-(OH)D levels through clinical evaluation of patients with osteoporosis.
To sum up the above findings, 44.4% of vitamin D deficient patients did not attain the optimal level of serum 25-(OH)D despite recommended daily intake of vitamin D to 1,000 IU in patients with osteoporosis. In the contrary, 88.9% of those patients attained optimal 25-(OH)D levels by doubling the recommended daily amount of vitamin D to 2,000 IU. Therefore, follow-up of serum 25-(OH)D levels for determining whether or not the optimal vitamin D levels were achieved may be required for vitamin D supplementation in vitamin D deficient patients with osteoporosis.
Notes
No potential conflict of interest relevant to this article was reported.