INTRODUCTION
Vitamin D is present in egg yolks, fish, and liver etc and partially obtained from sunlight exposure; ultraviolet (UV) rays provide a stimulus to skin when exposed to sunlight thereby synthesizing vitamin D. In addition, vitamin D is a hormone playing a significant role on bone and calcium metabolism. Vitamin D excess and deficiency can be evaluated by measuring 25-hydroxyvitamin D (25[OH]D; calcidiol, major circulating vitamin D).[1]
The diseases that may cause disorders on normal vitamin D metabolism, including chronic liver diseases, renal tubular disorders, and hereditary disorders caused by lack of sunlight exposure and vitamin D intake etc., are able to be the causes of skeletal disorders throughout entire body. Rickets is induced in case where these causes occur before physeal plate is closed. After physeal plate is closed, secondary hyperparathyroidism due to serious hypocalcaemia and osteomalacia due to disorders of bone mineralization are induced. For rickets and osteomalacia caused by vitamin D deficiency due to shortage in vitamin D intake and sunlight exposure, rickets caused by vitamin D deficiency occurred for children living in cities particularly because of lack of sunlight exposure as indoor lifestyle was preferred due to the industrial revolution.[2] However, it has been reported that rickets and osteomalacia that are caused by vitamin D deficiency are remarkably being decreased due to development of vitamin D supplements along with environmental changes. Recently, vitamin D deficiency gains attention again as prevalence of vitamin D deficiency increases even in young and healthy people because sunlight exposure is not enough due to telecommuting and indoor work environment and UV block has been excessively utilized.[3-5]
In Korea, there are osteomalacia cases caused by paraneoplastic syndrome due to tumor,[6,7] receptor resistance due to intake of anticonvulsants,[8] and Fanconi syndrome. [9] Only 2 cases have been reported regarding vitamin D deficiency caused by sunlight exposure and food intake as the present case pays attention.[10,11]
Lately, osteomalacia due to lack of sunlight exposure and vitamin D deficiency in a young male patient who stays indoor for months and maintains vegetarian diet for years were observed so that the authors would like to report the case with literature review.
CASE
Patient: 30-year-old, male
Chief complaint: walking disturbance, hip-joint pains, cramps in both pelvic limbs
Current medical history: The patient is vegetarian without any unusual medical history. He owns a private business; he usually transfers light objects within 10 kg. Since about 1-2 years ago, he had pain on his legs when walking and difficulties to run and walk up stairs. Also, he sometimes had cramps at hip-joint and hip muscles but he didn't experience much inconvenience in daily life. Three months before visiting a hospital, he did intensive work to carry things while moving so he had more serious pains at hip-joint part. Then the patient experienced difficulties in walking and abnormalities and oppressive pains around coccyx. He was disturbed while in sleep since he couldn't lie down due to the severe pains and cramps occurred as he spread his legs more. A half month before the hospital visit, he couldn't sleep due to serious cramps without specific reasons and then he came into neurology department out-patient clinic of the hospital in order to have additional examination and treatments.
Past history: The patient had no special past history such as hypertension, diabetes, hepatitis, and tuberculosis etc.
Family history: No one in his family had special past history including hypertension, diabetes, hepatitis, and tuberculosis etc. All family members (parents and five brothers and sisters) except for the patient are normal dieters who eat meats and had normal height and body weight.
Social history: The patient is a non-drinker and non-smoker. He is single and works at home as he owns his private business. He was reluctant to go out since his walking had changed. He didn't go out for about a year and he went out at night if necessary.
Systemic review and physical examination findings: In bio-vitality index from body examination, systolic blood pressure, diastolic blood pressure, pulse, breathing, and temperature were 118 mmHg, 58 mmHg, 84 times per minute, 20 times per minute, and 36.8℃, respectively. Height and body weight were 168.0 cm and 50.9 kg, respectively, the body weight had not been changed for several years. Deformation on upper pelvic limb or body was not observed. The patient claimed pains in both hip joints when walking or carrying heavy stuff. As he had pain like pulling behind of both legs when walking fast, he couldn't run and exhibited waddling gait. In neurologic examination, left and right were symmetric and strength index showed 4+, indicating slight muscle weakness.
Examination findings: In peripheral blood examination, leukocyte, hemoglobin, and thrombocyte were 8,100/mm3, 13.8 g/dL, and 268,000/mm3, respectively. In serum biochemical examination, total protein (7.9 g/dL), albumin (4.3 g/dL), blood urea nitrogen (15.9 mg/dL), creatinine (0.7 mg/dL), sodium (138 mmol/L), potassium (4.1 mmol/L), chlorine (102 mmol/L), and carbon dioxide (24 mmol/L) exhibited normal. Phosphorus (2.4 mg/dL; reference value 2.7-4.5), calcium (6.0 mg/dL; reference value 8.2-10.2), and ionized calcium (3.3 mg/dL; reference value 4.4-5.2) were decreased and alkaline phosphatase (313 U/L; reference value 35-129) was increased. Serum parathyroid hormone (268 pg/mL; reference value 13-54), 25(OH)D measured by radioimmunoassay (Diasorin kit) (less than 4.0 ng/mL; reference value 4.8-52.8), 1,25(OH)D (7.51 pg/mL; reference value 19.60-54.30), osteocalcin (32.9 ng/mL; reference value 11.3-37.0), N-telopeptide (NTx; 100 nMBCE/mMCr; reference value 14-81), urine calcium (0.6 mg/dL), and urine phosphorus (29.1 mg/dL) indicated vitamin D deficiency and secondary hyperparathyroidism.
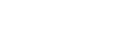
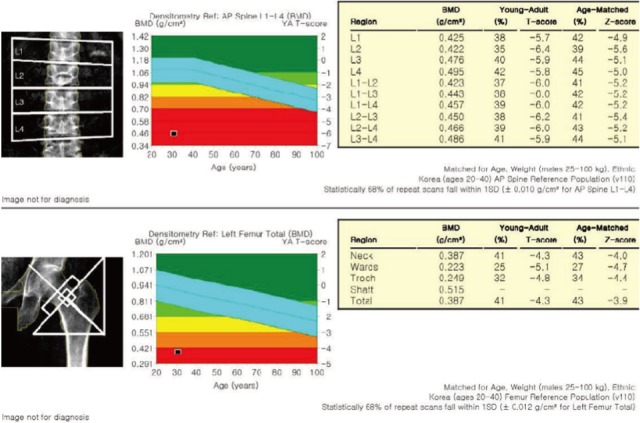
Radiologic examination findings: In spinal X-ray scanning, diffuse osteopenia was observed overall. Pseudofracture was not exhibited in femur, pelvic bone, and costal bone. In bone mineral density examination utilizing dual energy X-ray absorptiometry, severe diffuse osteopenia was observed with Z values of lumbar spine (L1-L4) (-5.4) and femoral neck (-4.0) (Fig. 1). In whole body bone scan, multiple increased uptakes including costal bone were exhibited and it was in agreement with the finding of osteomalacia (Fig. 2).
Clinical progress: In order to evaluate and find the causes of vitamin D deficiency in the patient, listening of medical history and environment investigation were carried out in detail. The patient had been vegetarian since 8 years ago; he had meals three times a day with general meals but he was vegan, the strictest type of vegetarian, who didn't eat meats, fish, eggs, and milk etc at all. He had a bowl of rice per meal and vegetables and legumes as side dishes. The patient hardly went out for the last 6 months and stayed and worked at home using internet. Therefore, we performed bone mineral density examination, serum hormone examination, and electrolyte examination in the patient who came into the hospital due to the walking impairment and were under examination in neurology department. Based upon the examination, the authors diagnosed osteomalacia caused by vitamin D deficiency due to undernutrition and lack of exposure to sunlight. The patient started taking calcitriol, 0.5 µg per day, and calcium carbonate, 1,000 mg per day. After a week, serum ionized calcium (4.0 mg/dL) and serum phosphorus (2.9 mg/dL) were observed to be increased. Serum ionized calcium was back to normal, 4.5 mg/dL, 12 days after the injection. As the patient got better after a week, bone biopsy was not carried out. We recommended him to have sufficient nutrition including vitamin D and to go out in order to be exposed to sunlight daily. The patient was prescribed calcitriol, 0.5 µg per day, and calcium carbonate, 1,000 mg per day, when he was discharged from the hospital. In follow up from out-patient clinic 3 months later, strength index, 5, was back to normal and pains at hip joint and walking impairment were improved. Serum calcium (8.7 mg/dL), phosphoric acid (4.3 mg/dL), ionized calcium (4.5 mg/dL), and 25(OH) D (5.9 ng/mL) were improved as well. Alkaline phosphatase and serum parathyroid hormone exhibited 391 U/L and 295 pg/mL, respectively.
DISCUSSION
Osteomalacia cases caused by tumors, liver diseases, and continuous anticonvulsants intake such as Phenobarbital etc were reported many times [6-9] but osteomalacia cases related to shortage of sunlight exposure or nutritional deficiency were rare in Korea. In Korea, Kim et al.[10] reported osteomalacia due to vitamin deficiency in a 59 year old male patient with chronic alcoholic liver disease and Myeong et al.[11] reported osteomalacia in a 36 year old female patient who was not exposed to sunlight for a long time.
The reasons why there are only small number of osteomalacia cases caused by vitamin D deficiency in adult are as follows; in case of osteomalacia, chronic vitamin D deficiency is preceded instead of the results from the short-term deficiency. Also, recently various vitamin D supplements are produced and many people take them. In addition, vegetarian diet and osteoporosis were reported more frequently in females than that of males and vitamin D deficiency in males is rare because males intake relatively more meats than that of females. As mentioned previously, even if vitamin D deficiency is present, osteomalacia caused by vitamin D is rare if there was enough sunlight exposure. Usually, males are exposed to sunlight more often than that of females so that the patient in the present case is very rare.
In Korea, only a case of vitamin D deficiency-induced osteomalacia was reported in a male patient with chronic alcoholic liver disease and internationally, osteomalacia cases caused by sunlight exposure and nutritional deficiency in a young male patient were not found in papers written in English.
Osteomalacia treatments can expect to have good results and prognosis by removing or improving the causes of diseases. Particularly, in case of osteomalacia caused by vitamin D deficiency and shortage of sunlight exposure, even though the deficiency is extended over a long period time, osteomalacia can be easily corrected if exposing to sunlight on a regular basis.
The patient in the present case had extreme lifestyle; he stayed at home so was not exposed to sunlight. He was vegetarian for 8 years so meats, eggs, milk, and fish etc were not included in his diet at all. Based upon the several examinations that we performed, the patient was diagnosed vitamin D deficiency-osteomalacia. Then, he had training with regards to vitamin D and calcium supplements prescription and sunlight exposure and then he was discharged from the hospital. Currently, the patient has outdoor activities frequently and is being changed to have various kinds of foods. The patient will be followed up through out-patient clinic periodically and administration of vitamin D and calcium is planned to be adjusted.
In the present case, more attention needs to be given on followings; 1) osteomalacia caused by vitamin D deficiency and lack of sunlight exposure can occur in young males 2) metabolic bone disease should be considered in the patients who was considered neurological abnormalities due to musculoskeletal impairments such as walking disturbance etc. Considering that osteomalacia can be prevented and treatment can be satisfactory only by correcting lifestyle, education and information regarding diets and lifestyle should be provided in social and public health point of view.
CONCLUSION
Osteomalacia mainly occurs in adults and is caused by various causes. It has been reported that osteomalacia caused by lack of sunlight exposure or vitamin D deficiency occurs relatively less frequent than that of in the past. Recently, however, lack of exposure of sunlight is very likely in modern life due to vegetarianism fever, vitalization of telecommuting, as well as indoor work; along with insufficient intake of meats and fish, osteomalacia is easily found via vitamin D deficiency.
We reported a case of osteomalacia that was caused by vitamin D deficiency due to vegetarian diet and shortage of sunlight exposure.

 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






