Effect of Sarcopenia on Postoperative Mortality in Osteoporotic Hip Fracture Patients
Article information
Abstract
Background
Few studies have investigated the effects of sarcopenia on postoperative outcomes including mortality rates following surgery for osteoporotic hip fractures. The purpose of the present study was to determine the prevalence of sarcopenia and the relationship between sarcopenia and 1- and 5-year mortality rates in a consecutive series of patients with osteoporotic hip fractures.
Methods
Among patients who underwent hip surgery for osteoporotic hip fractures, this study included 91 patients subjected to abdominal computed tomography within 1 year of hip surgery. We defined sarcopenia using sex-specific cut-off points for the skeletal muscle index at the level of the third lumbar vertebra. All patients were divided into 2 groups according to the presence or absence of sarcopenia and the 1- and 5-year mortality rates were compared. To confirm factors affecting mortality in addition to sarcopenia, we examined patient age, sex, American Society of Anesthesiologists grade, location of fracture, type of surgery, and bone mineral density.
Results
The 1- and 5-year mortality rates were 20.9% and 67.2%, respectively. Among the 45 patients with sarcopenia, the 1- and 5-year mortality rates were 22.2% and 82.7%, respectively. Of the 46 patients without sarcopenia, the 1- and 5-year mortality rates were 19.6% and 52.7%, respectively. Results of the Kaplan-Meier analysis showed that sarcopenia did not affect the 1-year mortality rate (P=0.793), but had a significant effect on the 5-year mortality rate (P=0.028). Both perioperative sarcopenia (P=0.018) and osteoporosis (P=0.000) affected the 5-year mortality rate.
Conclusions
Sarcopenia increases the risk of 5-year mortality in patients with osteoporotic hip fractures.
INTRODUCTION
Hip fractures of the elderly are frequently occurred by low energy trauma. Patients' age, comorbidity and severity of the injury are the factors affecting postoperative 1-year mortality rate.[1] In addition, half of survivors will develop permanent impairment in mobility and 10% to 20% of them would be hospitalized for readmission.[2] High mortality and morbidity rate of hip fractures will further increase the demand on both the individual and society.[3] Furthermore Korean National Health Insurance Service predicted that the incidence of osteoporotic fracture will increase as the elderly population increases, not only in Korea but around the world. It is estimated that the incidence will be doubled by 2050, so prevention and preparation are necessary.[4]
Sarcopenia is a syndrome characterized by loss of muscle mass and function with aging which increase risk of disability and death.[5] A few recent studies have shown that sarcopenia affects the mortality of abdominal surgery, as well as solid organ cancer surgery.[678] Several studies have identified factors affecting mortality after hip surgery such as sex, age, type of fracture, and preoperative condition.[9] And, the effect of sarcopenia on mortality rate after hip surgery has been presented for a relative short-term mortality rate.[10]
Thus, the purpose of this study is to investigate the prevalence of sarcopenia and its effect on short-term and mid-term mortality rates after hip surgery in osteoporotic hip fracture patients. The hypothesis of this study is that sarcopenia would present in a substantial proportion of patients with osteoporotic hip fracture and sarcopenia would affect postoperative mortality.
METHODS
1. Subjects
This study complies with the Declaration of Helsinki and was performed according to ethics committee approval. From January 2006 to May 2013, we evaluated 388 patients over 65 years of age who were diagnosed with fresh hip (femur neck or intertrochanteric) fracture and who underwent operative treatment. Then, for evaluation about perioperative sarcopenia, 125 patients who performed abdominal computed tomography (CT) within 1 year before hip surgery were selected. Patients were excluded for any of the following: (1) not performed dual energy X-ray absorptiometry (DXA); (2) T-score >−2.5 on DXA; (3) bilateral hip fracture; (4) possibility of the effects on mortality rate including solid organ malignancies detected via abdominal CT. Finally, a total of 91 patients were finally included in this study. The 91 patients were divided into 2 groups according to the presence or absence of sarcopenia. A flow chart of study subjects are shown in Figure 1. Censoring was based on the last follow-up date if mortality events were due to other reasons such as traffic accident, or if the time of mortality event was not clear due to follow-up loss. The medical records of the patients were retrospectively reviewed for basic data such as sex, age, weight, height, location of fracture, type of surgery, operation record and other patient records.
2. Sarcopenia assessment
The diagnostic criteria for sarcopenia vary from literature to study, so there is some controversy. We defined sarcopenia by using a sex-specific cut-off points for skeletal muscle index (SMI) at the level of third lumbar (L3) vertebra. The L3 vertebra region is closely related to the distribution of whole body muscles and may be an important index for measuring the amount of muscle in the body.[11] The L3 SMI (cm2/m2) was calculated dividing the skeletal muscle area (SMA) at L3 vertebra region by the square of height (cm2). In previous studies, the SMA was measured at the level of L3 to identify sarcopenia, including paraspinal muscle, psoas muscle, and abdominal wall muscle.[12] The SMA was measured using a picture archiving and communication system (PiViewSTAR 5.0; INFINITT, Seoul, Korea). Two adjacent axial images within the same series were used to determine the cross-sectional area of L3 skeletal muscle, and the mean of the 2 measurements was calculated for each patient. A single trained staff person corrected the boundary of the entire area of L3 skeletal muscle. Rather than using the cut-off values for sarcopenia for men (<52.4 cm2/m2) and women (<38.5 cm2/m2) that have been used Western countries,[13] we employed the adjusted criteria for the Korean population (male, <42.2 cm2/m2; female, <33.9 cm2/m2).[14] A patient with a value below these was diagnosed as sarcopenia.
3. Overall mortality rate and associated factors
The overall 1- and 5-year mortality rates of patients undergoing hip fracture surgery were obtained. Mortality was identified from hospital records or by interviewing a member of the family of the patient involved. To confirm factors affecting 5-year mortality rate after hip surgery in addition to sarcopenia, we checked patients' age, sex, American Society of Anesthesiologists (ASA) grade, location of fracture, type of surgery and bone mineral density (BMD). The ASA grade (grade 1–6) was confirmed by an anesthesiologist at our institution to confirm the objective preoperative health status. Locations of fracture were femur neck or intertrochanter and types of surgery were closed reduction-internal fixation (CRIF) or arthroplasty surgery (hemiarthroplasty or total hip arthroplasty). BMD was measured approximately 1 week after surgery using DXA and the mean T-score was assessed.
4. Statistical analysis
Statistical analysis was performed with SPSS version 21.0 (SPSS Inc., Chicago, IL, USA). A P-value of less than 0.05 was considered significant. We used a χ2 test to assess differences in categorical variables and a t-test or analysis of variance test for numerical variables. All reported P-values were 2-sided, and a P-value of less than 0.05 was used to determine significance. For evaluation of mortality rate, Kaplan-Meier analysis was used for survival curves, and log-rank tests were used to assess significance. The impact of perioperative sarcopenia on overall mortality rate was examined using Cox proportional hazard models. First, multivariable Cox regression analysis was performed with all potential variables. Then, variables not significantly contributing to the fit of the model were removed from the model using a backward selection method. Statistical analyses were carried out using SPSS for Windows software (version 22.0; SPSS Inc.). A P-value of less than 0.05 was considered significant.
RESULTS
1. Subjects
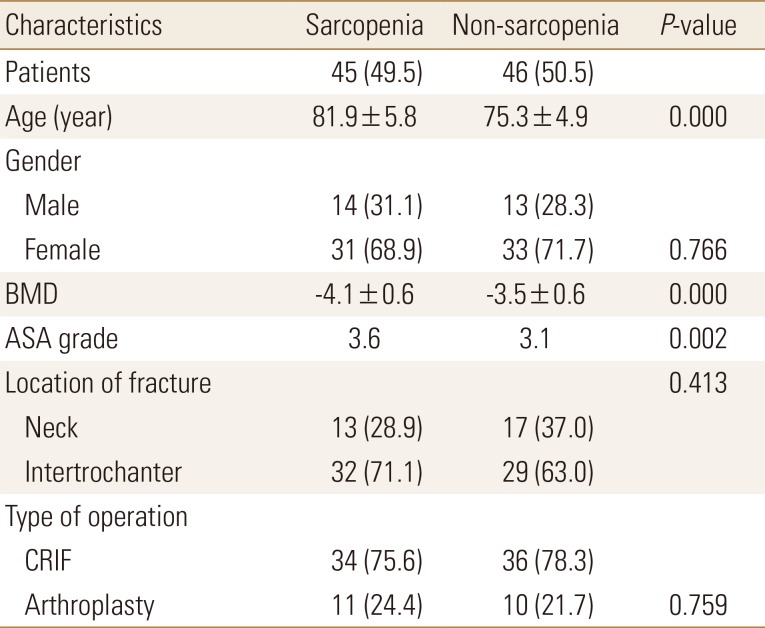
A total of 388 patients underwent osteoporotic hip fracture surgery and preoperative abdominal CT was performed in 125 patients. Thirty-four patients were excluded for the exclusion criteria mentioned above. A total of 91 patients were finally included in this study. Of the 91 patients, 27 were males and 64 were females. The mean age of the patients at the time of surgery was 78.5 years (range, 65–94 years). Thirty patients (33.0%) had femoral neck fractures, and 61 patients (67.0%) had femoral intertrochanteric fractures. Seventy patients (76.9%) underwent CRIF surgery, and 21 patients (23.1%) underwent arthroplasty surgery. Mean ASA grade was 3.6 (range, 2–6). BMD was an average T-score of −3.81 (range, −2.6~−5.2). Of 91 patients, 45 (49.5%) were diagnosed with sarcopenia. The mean age of this group was 81.9 years, and 14 were males and 31 were females. Among 46 (50.5%) who didn't have sarcopenia, the mean age of this group was 75.3 years, and 13 were males and 33 were females. Detailed data of the patients are listed in Table 1.
2. Mortality rate
1) Overall mortality rate
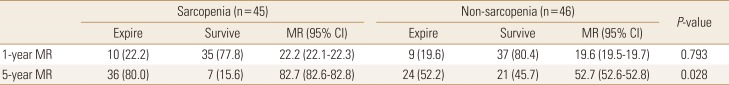
Among the total of 91 patients, 19 patients died before 1 year after surgery, and 1-year mortality rate was 20.9% (95% confidence interval [CI], 20.8–21.0). Five years after the surgery, 60 out of 91 patients expired and the 5-year mortality rate was 67.2% (95% CI, 67.1–67.3).
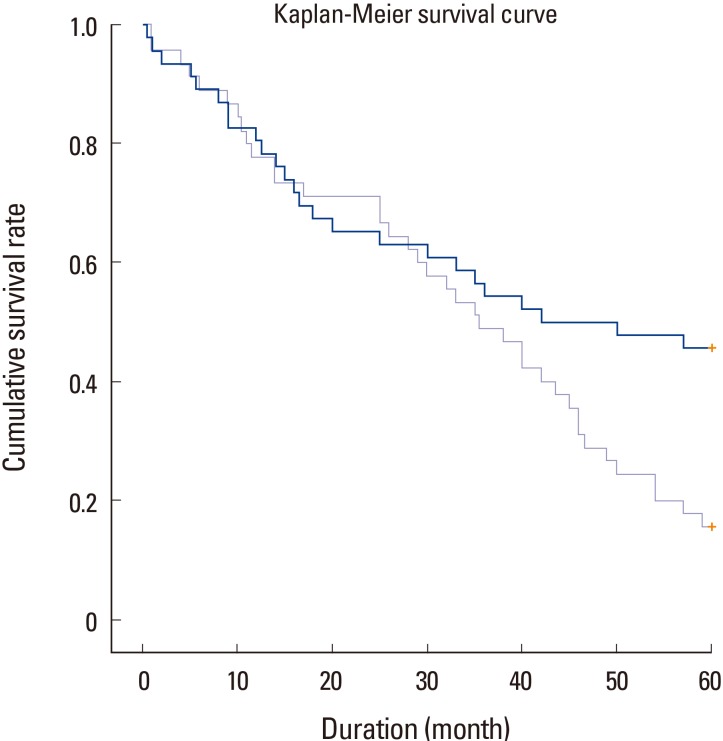
2) Mortality rate according to presence of sarcopenia
The 1-year mortality rate was 22.2% in the group with sarcopenia and 19.6 in the group without sarcopenia. There was no statistically significant difference in the 1-year mortality rate between the 2 groups (P=0.793). The 5-year mortality rate was 82.7% in the group with sarcopenia and 52.7% in the group without sarcopenia (Table 2). There was a statistically significant difference in 5-year mortality rate between the 2 groups (P=0.028) (Fig. 2).
3) Factors affecting to 5-year mortality rate - Cox regression analyses
Correlation between 5-year mortality and related factors were statistically analyzed and the results were obtained. Multivariable Cox analysis including all predictors showed that perioperative sarcopenia (hazard ratio [HR], 3.998; 95% CI, 1.798–8.889), BMD (HR, 5.435; 95% CI, 2.457–12.025) and age (HR, 1.113; 95% CI, 1.002–1.236) significantly associated with 5-year mortality rate after hip surgery. On multivariable analysis using a backward selection method, perioperative sarcopenia (HR, 2.144; 95% CI, 1.140–4.031) and BMD (HR, 8.441; 95% CI, 4.841–14.720) remained as significant risk factors for increased mortality rate after hip surgery (Table 3).
DISCUSSION
Osteoporosis and sarcopenia are common in older age and associated with significant morbidity and mortality. Consequently, they are both attended by a considerable socioeconomic burden. There is also evidence of a mechanistic interrelationship between muscle and bone with sarcopenic individuals at greater risk of osteoporosis and vice versa.[15] Our findings confirm that the facts above also apply to osteoporotic hip fracture patients. As a result of this study, sarcopenia didn't affect the 1-year mortality rate after hip surgery, but sarcopenia and osteoporosis affected the 5-year mortality rate. The result verifies that sarcopenia and osteoporosis are important factors to affect the mid-term survival after hip fracture surgery. While age and ASA grade are factors that cannot be compensated by patients, sarcopenia and osteoporosis are conditions that could be overcome with the patient's personal will and effort, which could be an effective way to reduce long-term mortality after hip surgery. This important point seems to give the message that the Korea society that has already entered the aged society should actively educate the people about it. Although we can't clearly explain the different effects of sarcopenia on 1-year mortality and 5-year mortality because it is not possible to pinpoint the cause of the patient's death, functional ambulation is thought to play an important role in long-term prognosis including mortality rate after hip fracture surgery.
In recent studies, hip fractures have been reported to have a high mortality rate of 14% to 36% within 1 year postoperatively and are directly related to mortality.[1617] In our study, 1-year total mortality rate was 20.9%, similar to other studies. While previous studies reported only 1- or 2-year mortality rate after surgery, we were able to report the 5-year mortality rate (67.2%) which is relatively long-term period.
Owens et al.[18] demonstrated statistically significant relation between ASA grade and mortality, which is consistent in this study. In the study of White et al.[19], preoperative ASA grade >3 with severe comorbidities showed statistically higher 1-year mortality rate, showing that a patient's comorbidities has a greater impact on mortality rate than age. In other several studies, preoperative health status has been found to be an important factor in the patient's mortality as well. Our results also suggest that preoperative ASA grade affects 5-year mortality rate.
Kenzora et al.[20] and Miller [21] reported that mortality increased with age. On the other hand, White et al.[19] and Cornwall et al.[22] found there was no difference in the mortality rate by age. In this study, the postoperative 5-year mortality rate was increased with age. As age increased, the prevalence and degree of osteoporosis and sarcopenia are thought to increase.
Miller [21] reported that men had a high mortality rate, while Kenzora et al.[20] reported no difference in mortality by gender, and there are several studies in Korea that support both claims.[232425] In this study, gender of patient did not affect 5-year mortality.
The main strength of this study is that several studies have reported the association of sarcopenia with hip fracture mortality, but most have been short-term mortality of about one year,[926] but this study analyzed the 5-year mortality. On the other hand, this study has some limitations. First, study design was retrospective and small subject number, so there can be a selection bias and sarcopenia was diagnosed retrospectively only by muscle mass. Function and gait speed were not be assessed in this study. Therefore, we may have underestimated the number of patients with sarcopenia by classifying those with decreased muscle function as normal. Second, performance, such as the possibility of ambulation and the activities of daily living, were not included when evaluate the outcomes of hip surgery. Although we tried to evaluate the patient's performance through questionnaires, there were limitations as most of the patients were suffering from cognitive impairment. Third, ASA grade could not fully represent patient's medical comorbidity. Therefore, a prospective follow-up study is needed. Fourth, the causality between hip surgery and mortality is unclear as cause of death was not analyzed.
CONCLUSIONS
Prevention of sarcopenia and osteoporosis through regular exercise and appropriate management is considered to be an important correctable factor in lowering the mortality rate after hip surgery. And above all, prevention of hip fracture is important.
Notes
No potential conflict of interest relevant to this article was reported.