 |
 |
| jbm > Volume 24(2); 2017 > Article |
|
Abstract
Background
The present study estimated healthcare costs of osteoporotic fractures including spine, hip, distal radius and humerus in Koreans over 50 years of age using national claims data.
Methods
Korea National Health Insurance data between 2008 and 2011 was searched for all claims records of outpatient visits or hospital admissions of patients ≥50-year-of-age. Osteoporosis-related fractures were identified using certain the International Classification of Diseases, Tenth Revision codes and site-specific physician claims for procedures in a patient age cut-off value of 50 years. The healthcare costs included acute phase costs accounting for emergency medical care given immediately after fracture, costs due to further hospitalization and surgical procedures, physiotherapy sessions according to the site of the fracture, and outpatient visits in the year after discharge.
Results
The total estimated healthcare costs of osteoporotic fractures in 2011 was $722 million. From 2008 to 2011, the total number and healthcare costs of osteoporotic fractures increased 28.9% (from 127,070 to 163,823) and 31.6% (from $549 million to $722 million), respectively. The portion of national health care expenditure was ranged from 2.3% in 2008 to 2.2% in 2011. The mean healthcare cost of osteoporotic fractures per person increased 2.1% from $4,321 in 2008 to $4,410 in 2011.The mean healthcare costs were highest for hip fractures followed by spine, humerus, and distal radius fractures.
Osteoporosis is a common condition that makes low trauma fractures more likely. Osteoporosis-related fractures including spine, hip, wrist, and humerus are important causes of morbidity, disability, and mortality in elderly patients, and also increases the economic burden of health care.[1,2,3] Although the incidence of major osteoporotic fractures has remained steady or declined in western industrialized countries during the last decade,[4,5,6] the total number of osteoporotic fractures is still increasing. Other countries are reporting increasing trend of osteoporotic fractures. [7,8]
South Korea became an aging society (elderly population ≥7% of the total population) in 2000. In 2018, South Korea will become an aged society (defined as an elderly population ≥14% of the total population), and by 2026 will be a super-aged society (elderly population ≥20% of the total population). This will increase the proportion of the population with age-related frailty. A higher prevalence of osteoporotic fractures is anticipated. In South Korea >50-year-of-age, 59.5% of women and 23.8% of men will experience osteoporosis-related fractures.[9] This will impose increasing economic and healthcare burdens.
Several studies regarding cost of osteoporotic fractures have been reporting and emphasizing excess costs for their fractures, however the situation for South Korea is unclear. The present study was undertaken to estimate healthcare costs of osteoporotic fractures including spine, hip, distal radius and humerus in Koreans over 50 years of age using national claims data from 2008 to 2011 and to compare findings with other studies.
The Korean National Health Insurance (KNHI) covers 100% of the population including 97% health insurance and 3% medical aid.[3] All information about the volume and burden of diseases can be obtained from this centralized database, with the exception of procedures that are not covered by insurance, such as cosmetic surgery or traffic accidents, which are covered by commerical insurance. All clinics and hospitals submit data on inpatients and outpatients including data on diagnosis and medical costs for claims purposes. KNHI data include information on date of discharge and discharge diagnoses (both principal diagnoses and additional diagnoses) that are assigned exclusively by the physician at discharge according to the International Classification of Diseases, Tenth Revision (ICD-10). The advantage of using osteoporotic fracture study data from KNHI is that high-energy trauma fractures, such as from traffic or industrial accidents, are automatically excluded since their costs are covered by different insurance systems. In this study, the complete paid claims data and eligibility files were merged to create a database consisting of data for all filled prescriptions, procedures, outpatient physician encounters, and hospitalizations. All traceable personal identification numbers were transformed into anonymous codes.
KNHI data colletced between January 1, 2008 and December 31, 2011 were searched to identify all claims records of outpatient visits or hospital admissions of patients ≥50-year-of-age. Osteoporosis-related fractures were identified using certain ICD-10 codes and site-specific physician claims for procedures.[10,11,12,13] Fractures were identified on the basis of selected ICD-10 codes for hip (ICD-10 codes S72.0 [fracture of the femoral neck], S72.1 [pertrochanteric fracture] and seven procedures [open reduction of fractured extremity-femur, closed pinning-femur, external fixation-pelvis/femur, closed reduction of fractured extremity-pelvis/femur, bone traction, skin traction, hemiarthroplasty-hip]); spine (S22.0 [fracture of the thoracic spine], S22.1 [multiple fractures of the thoracic spine], S32.0 [fracture of the lumbar spine], M48.4 [fatigue fracture of vertebra] and M48.5 [collapsed vertebra]); distal radius (S52.5 [fracture of the distal radius] and S52.6 [combined fracture of the distal radius/ulna]); humerus (S42.2 [fracture of the proximal humerus] and S42.3 [fracture of shaft of humerus]); and overall fractures.[9] The date of earliest qualifying fracture code was considered the index date. An incident fracture was identified if there was one hospitalization or two physician visits (within 6-month) with the relevant diagnosis code, provided that this was preceded by a 6-month period (washout) without any codes for the same diagnosis. To exclude treatment costs of other severe diseases, patients who were diagnosed with organ transplantation, chronic renal failure, and other severe diseases were excluded. The total number of men and women >50-year-of-age in the Korean population was obtained on 23 August 2010 from the web site of the Statistics Korea (http://www.kosis.kr/), which is the central government organization for statistics.
We estsimated direct healthcare costs based on an insurance
perspective. The healthcare costs are expenditures spent on the medical procedures and services associated with treatment performed in hospitals or clinics. These include costs for hospitalization, outpatient visits, and prescription drugs. The health insurance claims data were analyzed to calculate both outpatient and inpatient costs related to osteoporotic fractures. Claims amount for the first visit and for the follow-up treatments for 1 year were tallied for each patient. When clinics and hospitals manage insured patients, they request reimbursement of medical costs from the KNHI at the end of each month. As the KNHI program covers osteoporosis and its related diseases, nearly all cases of osteoporotic fracture were covered in this analysis. For drug expenditures, inpatient costs already included drug costs incurred during hospitalization. Outpatient drug expenses were calculated using the proportion of outpatient, and inpatient-outpatient drug costs provided in the annual National Health Insurance Service (NHIS) statistical report. Because there is only one insurance system in Korea, KNHI claims data are nationally representative of medical care costs covered by the Korean insurance program. However, KNHI claims data do not include non-covered costs, such as for assistive devices, caregivers, and over the counter (OTC) drugs. All costs were first calculated in Korean Won (KRW) and then converted to United States dollars (USD) by using the 2011 year average conversion rate of 1,107 KRW per 1 USD (http//ecos.bok.or.kr/).
Bewteen the 2008 and 2011, of 690,439 osteoporotic fractures, 97,932 (14.2%) osteoporotic fracture were excluded due to patients who were diagnosed with organ transplantation, chronic renal failure, and other severe diseases. Therefore, 592,507 of osteoporotic fractrures were included. The total number of all osteoporotic fractures among Koreans ≥50-year-of-age increased 28.9% (from 127,070 to 163,823) The largest increase in the number of fractures was distal radius fracture (31.6%) and then spine fracture (29.5%). All osteoporotic fractures increased by 6.6% per year (Table 1). The age adjusted incidence of osteoporotic fractures increased from 1,127/100,000 in 2008 to 1,295/100,000 in 2011, and the gender specific incidence was increased by 14.1% in men and 16% in women (Fig. 1).
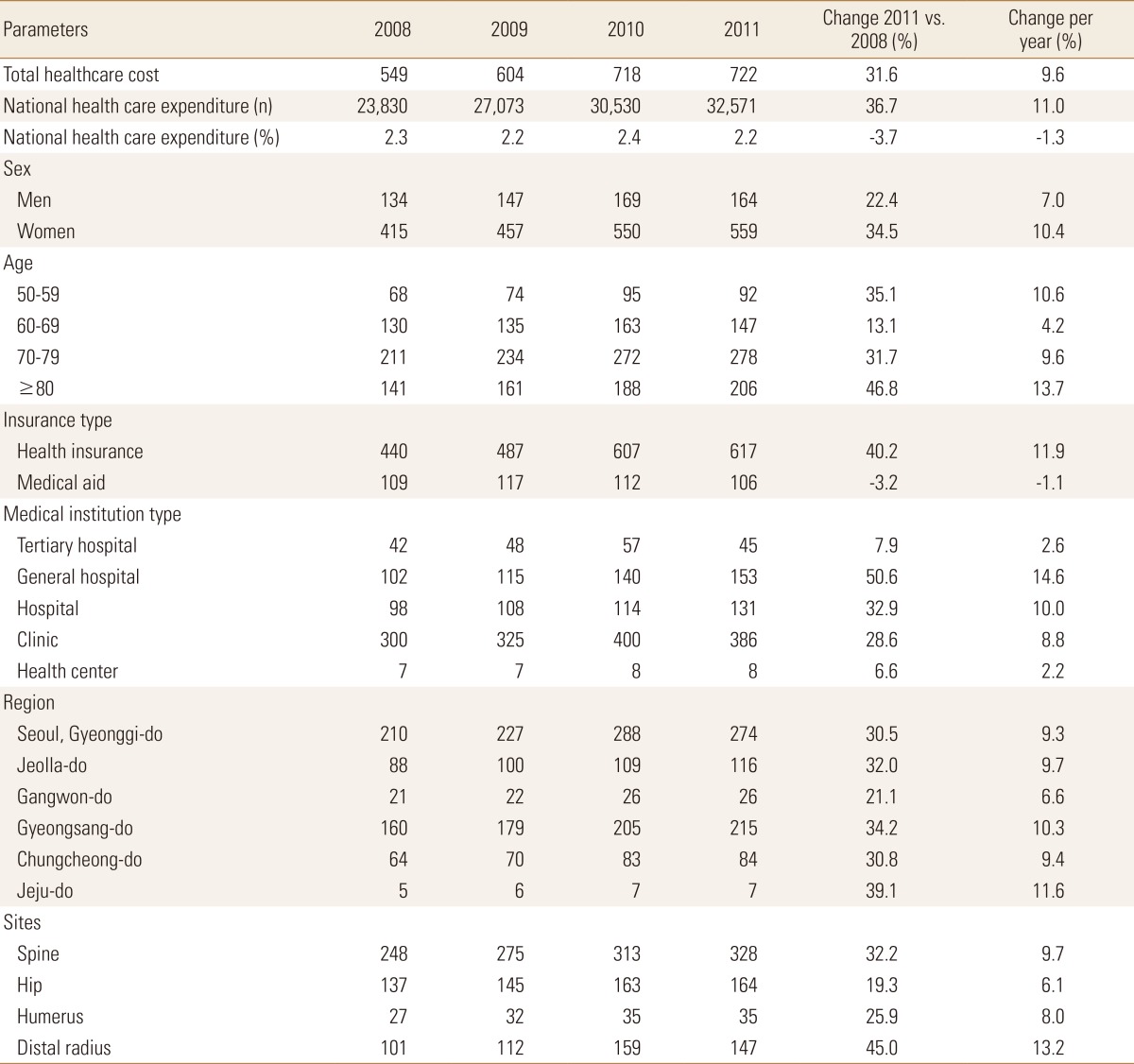
Consistent with increases in the absolute number of fractures, total healthcare costs during the 12 months following the osteoporotic fracture increased by 22.4% in men and 34.5% in women over 4 years. The proportion of national health care expenditures was steady from 2.3% in 2008 to 2.2% in 2011 (Table 2).
In 2011, the total estimated healthcare costs of osteoporotic fractures was $722 million, of which $559 million (77.3%) was for the treatment of women and $164 million (22.7%) for men.
The mean healthcare cost per patient was increased 2.1% from $4.321 in 2008 to $4,410 in 2011 (Table 3). Resource use data in 2011 indicated that hospitalization accounted for $480 million (66.5%) of this expense, followed by outpatient care ($127 million, 17.6%) and drug therapy ($116 million, 15.9%). The estimated cost of hospitalization, outpatient, and drug therapy was increased by 28.7%, 39.8%, and 35.3%, respectively, during the study period (Fig. 2).
Although the total number and healthcare costs of osteoporotic fractures in men were 4 times and 3 times lower than in women, respectively, the mean healthcare cost in men was 1.2 times higher than in women during the study period (Table 2 and 3).
Compared by age, the total healthcare costs increased in people aged 50 to 79 years and decreased thereafter. However, the mean healthcare cost ≥80-year-of-age was 1.9 times higher than for patients in their 50s. According to insurance type, as expected, the total healthcare cost of the medical insurance system was 4 to 6 times higher than the medical aid system. But, the mean healthcare cost was unexpectedly higher in patient reimbursed by the medical aid system. As expected, total healthcare costs were highest in clinic, followed by general hospital. According to regional classification, total health care cost was highest in Seoul and Gyeonggi-do, followed by Gyeongsang-do, Jeolla-do, Chungcheong-do, Gangwon-do, and Jeju-do. However, mean healthcare cost was highest in Jeolla-do, followed by Gyeongsang-do.
Concerning anatomical classifications, although total healthcare costs were highest for spine fractures, followed by hip fractures, distal radius fractures, and humerus fractures. Mean healthcare costs were highest for hip fractures, and followed by spine fractures, humerus fractures, and distal radius fractures.
The mean healthcare costs in 2011 were $4,512 for spine fractures, $8,302 for hip fractures, $3,893 for humerus fractures, and $2,591 for distal radius fractures.
Increased in total healthcare costs were evident for all fracture types with the largest percentage increase in distal radius fractures (45%) and spine fractures (32.2%) increase. Although total healthcare cost of hip fractures increased by 6.1% per year, mean healthcare costs decreased by 0.4% per year (Table 2 and 3).
The present data clarify the economic burden in South Korea of osteoporotic fractures including spine, hip, distal radius, and humerus fractures. This information has been widely reported elsewhere, but his is the first study of the nationwide healthcare costs of osteoporotic fractures in South Korea and these results are expecting general population and government officials will increase the attention to osteoporosis and related fractures.
A continuous increase in the national fracture trend and the annual costs for osteoporotic fractures over the 4 years study period between 2008 and 2011 was evident in men and women. During this time, the number of osteoporotic fractures increased by 28.9% and the total healthcare cost increased by 31.6%. Total healthcare costs of osteoporotic fracture steeply increased from $549 million in 2008 to $722 million in 2011. The total cost in 2011 included $559 million for women and $164 million for men. Concerning the cost depending on the type of fracture, the most expensive fracture for both genders was spine fracture, accounting for 43% to 45% of the total costs.
These findings are inconsistent with other reports. In Denmark, the total cost of osteoporotic fractures was estimated to €1.563 billion in 2011, at €628 million and €936 million for men and women, respectively.[14] The most expensive fracture was first hip fracture accounting for 20% to 38% of the total costs. In the US, the direct cost burden of all osteoporotic fractures was estimated at $16.9 billion in 2005.[15] Total cost distribution by fracture type revealed that hip fractures accounted for 72% of the total cost (but only 14% of fracture), followed by other fractures (14%), spine fractures (6%), pelvic fractures (5%), and wrist fractures (3%). In our study, the overall distribution of incident fractures revealed that spine fractures comprised the largest share (43-46%), followed by distal radius fractures (32-37%), hip fractures (12-13%), and humerus fractures (5-6%). The proportion of spine fractures in our study was higher than in the other studies.
For spine fractures, the true prevalence is expected to be underestimated, since the majority are asymptomatic and morphometric.[16] Because of the difference in health insurance system between nations (KNHI covers 100% of the population), the numbers identified by diagnosis codes in other country might represent the minority of spine fractures.
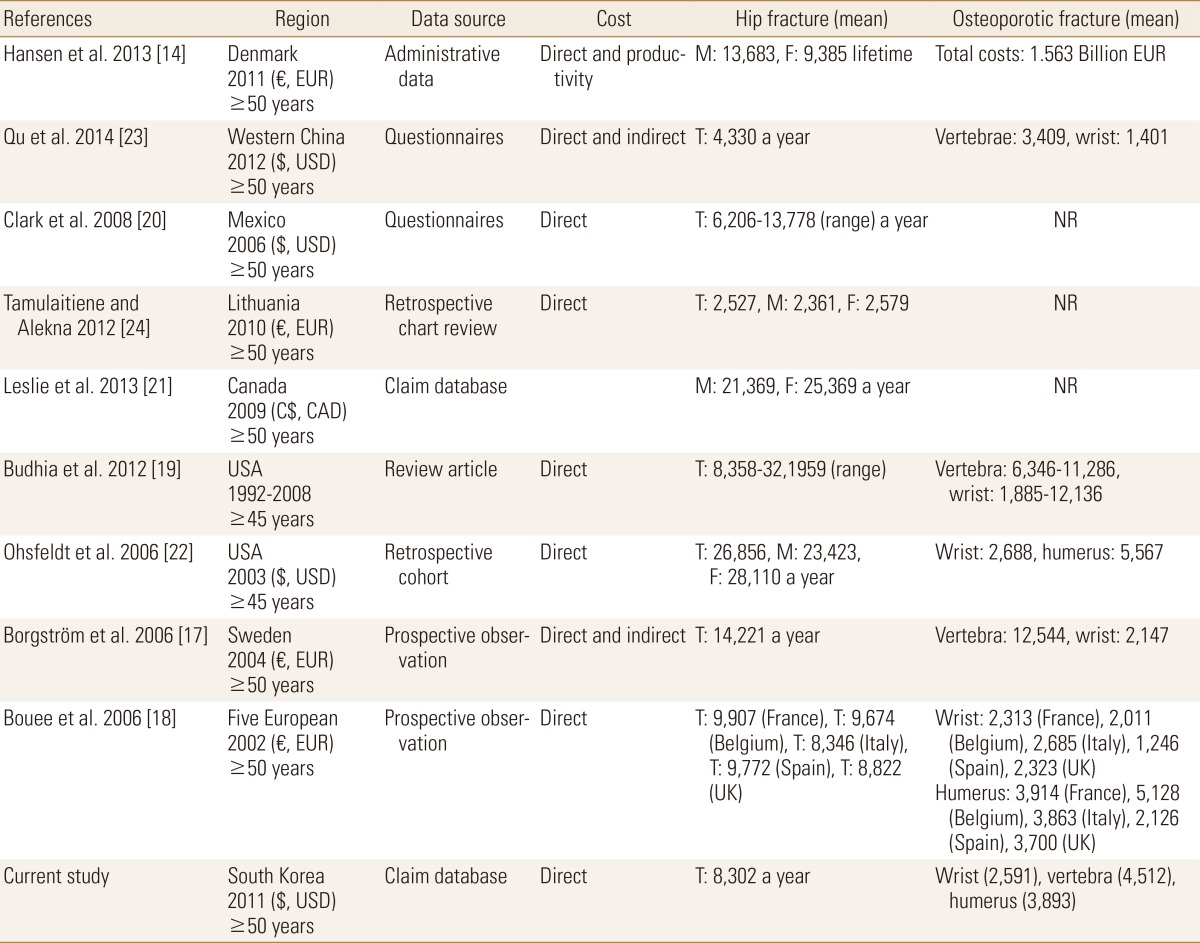
Presently, the mean healthcare cost in 2011 was estimated as $4,410; mean cost was highest for hip fractures ($8,302), followed by spine fractures ($4,512), humerus fractures ($3,893), and distal radius fractures ($2,591). The costs of hip fractures are notoriously highest among osteoporotic fractures. The costs of osteoporotic hip fractures have been amply studied.[14,17,18,19,20,21,22,23,24] The mean cost of hip fractures is difficult to compare between the present and prior studies due to differences in study year, study region, evaluation methods, size of population investigated, different age groups, and data presentation. With that caveat, a summary of mean healthcare costs of hip fractures is presented in Table 4. The mean cost of hip fracture in Korea is higher than those in China, Lituania, and Mexico, but is considerably lower than in the United States and many European countries. A 2012 study based in western China reported that the mean cost was highest in hip fractures ($3,688), followed spine fractures ($2,774), and wrist fractures ($1,166). [23] In the US, the mean cost of hip fractures ranged from $8,358-$32,195, followed by spine fractures (range, $6,346-$11,286), and wrist and forearm fractures (range, $1,885-$12,136).[19]
Although the total cost of osteoporotic fractures was higher in women than men, the mean cost of osteoporotic fractures in men was more expensive than in women. The higher total costs in women were caused by higher incidence of osteoporotic fractures than in men. Therefore, to decrease the economic burden of osteoporotic fracture, an active intervention strategy should be established to manage fracture related risk factors in osteoporotic women. The present mean cost data are inconsistent with other studies. A study from Denmark reported similar findings, with the estimated average incremental costs imposed by osteoporotic fractures for men and women ≥50-year-of-age in 2011 was €35,714 and €26,152 per person, respectively. Although women consumed the highest total cost, men on average were more expensive than women because more women are at risk of developing osteoporosis (40.8% vs. 17.7%).[14,25] However, in the US, the mean cost of osteoporotic fractures in women was higher than in men.[22] The US study evaluated the fragility fracture-related direct medical costs during the first year following a nonvertebral fracture in a managed care setting. The mean costs per fracture per year for all nonvertebral fractures were $11,013 in women and $10,593 in men.[22]
It is worth comparing the total cost of osteoporotic fracture with that due to other diseases to help understand the relative economic impact of osteoporotic fracture. The annual insurance-covered medical cost of osteoporotic fracture in our study ($722 million in 2011) was higher than the direct medical costs for acute myocardial infarction ($607 million in 2012).[26] On the basis of these results, the relative scale of osteoporotic fracture costs can be predicted, which highlights the need for prevention and management strategies for osteoporotic fractures. By comparing the estimated economic burden of multiple diseases, government officials can make informed decisions about the allocation of resources to service provision, prevention strategies, and research funding.
The study had several limitations. First, only the direct healthcare costs covered by insurance were assessed. Non-medical costs, such as over-the-counter products or herbal medicines, transportation costs, and caregiver costs, as well as indirect costs including lost productivity were not evaluated. Considering that many Korean patients at risk of fracture use herbal medicines for musculoskeletal symptoms, the potential medical costs of osteoporotic fractures could be substantially greater than shown. Further studies that include non-medical and indirect costs might be necessary to evaluate the economic burden of osteoporotic fractures in South Korea. Second, the quality of life was not been estimated or valued for this study population. If these costs were considered, the economic burden due to osteoporotic fracture could be even higher. Third, to minimize overestimation of direct cost of osteoporotic fracture, 97,932 (14.2%) of osteoporotic fracture who had concomitant diseases such as organ transplantation, chronic renal failure, and other severe diseases were excluded. Therefore, direct costs in this study are possible to underestimate. Finally, direct comparison between the data regarding cost of osteoporotic fractures was nearly impossible because of differences in study duration, study region, size of population investigated, different age groups, data presentation and study designs.
Total healthcare costs of osteoporotic fractures in South Korea was estimated using nationally representative KNHI data and determined to be $722 million, the equivalent of 2.2% of the national health care expenditure in 2011. The total healthcare cost of osteoporotic fractures has increased by 6.6% per year from 2008 to 2011. Considering the rapid aging in the South Korean population, the economic burden of osteoporotic fractures will be an ongoing important health problem in elderly population. Therefore, public health strategy preventing osteoporotic fractures to minimize the economic burden would be prudent.
ACKNOWLEDGEMENTS
National Health Insurance Database was provided by the National Health Insurance Service (NHIS) of Korea. The authors would like to thank the National Health Insurance Service for cooperation. This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Korea (grant number: HI13C1522 and HC15C1189). This study was supported by research funding from Korean Society for Bone and Mineral Research.
References
1. Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int 2005;16(Suppl 2):S3-S7.



2. Lee SR, Ha YC, Kang H, et al. Morbidity and mortality in Jeju residents over 50-years of age with hip fracture with mean 6-year follow-up: a prospective cohort study. J Korean Med Sci 2013;28:1089-1094.



3. Yoon HK, Park C, Jang S, et al. Incidence and mortality following hip fracture in Korea. J Korean Med Sci 2011;26:1087-1092.



4. Lix LM, Azimaee M, Osman BA, et al. Osteoporosis-related fracture case definitions for population-based administrative data. BMC Public Health 2012;12:301




5. Siggeirsdottir K, Aspelund T, Jonsson BY, et al. Epidemiology of fractures in Iceland and secular trends in major osteoporotic fractures 1989-2008. Osteoporos Int 2014;25:211-219.



6. Cassell E, Clapperton A. A decreasing trend in fall-related hip fracture incidence in Victoria, Australia. Osteoporos Int 2013;24:99-109.



7. Sakuma M, Endo N, Oinuma T, et al. Incidence of osteoporotic fractures in Sado, Japan in 2010. J Bone Miner Metab 2014;32:200-205.



8. Johansson H, Clark P, Carlos F, et al. Increasing age- and sex-specific rates of hip fracture in Mexico: a survey of the Mexican Institute of Social Security. Osteoporos Int 2011;22:2359-2364.



9. Park C, Ha YC, Jang S, et al. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J Bone Miner Metab 2011;29:744-751.



10. Ha YC, Kim TY, Lee A, et al. Current trends and future projections of hip fracture in South Korea using nationwide claims data. Osteoporos Int 2016;27:2603-2609.



11. Kim TY, Jang S, Park CM, et al. Trends of incidence, mortality, and future projection of spinal fractures in Korea using nationwide claims data. J Korean Med Sci 2016;31:801-805.



12. Kwon GD, Jang S, Lee A, et al. Incidence and mortality after distal radius fractures in adults aged 50 years and older in Korea. J Korean Med Sci 2016;31:630-634.



13. Park C, Jang S, Lee A, et al. Incidence and mortality after proximal humerus fractures over 50 years of age in South Korea: national claim data from 2008 to 2012. J Bone Metab 2015;22:17-21.



14. Hansen L, Mathiesen AS, Vestergaard P, et al. A health economic analysis of osteoporotic fractures: who carries the burden? Arch Osteoporos 2013;8:126




15. Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 2007;22:465-475.


16. Boonen S, Singer AJ. Osteoporosis management: impact of fracture type on cost and quality of life in patients at risk for fracture I. Curr Med Res Opin 2008;24:1781-1788.


17. Borgström F, Zethraeus N, Johnell O, et al. Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int 2006;17:637-650.



18. Bouee S, Lafuma A, Fagnani F, et al. Estimation of direct unit costs associated with non-vertebral osteoporotic fractures in five European countries. Rheumatol Int 2006;26:1063-1072.



19. Budhia S, Mikyas Y, Tang M, et al. Osteoporotic fractures: a systematic review of U.S. healthcare costs and resource utilization. Pharmacoeconomics 2012;30:147-170.


20. Clark P, Carlos F, Barrera C, et al. Direct costs of osteoporosis and hip fracture: an analysis for the Mexican healthcare system. Osteoporos Int 2008;19:269-276.



21. Leslie WD, Lix LM, Finlayson GS, et al. Direct healthcare costs for 5 years post-fracture in Canada: a long-term population-based assessment. Osteoporos Int 2013;24:1697-1705.



22. Ohsfeldt RL, Borisov NN, Sheer RL. Fragility fracture-related direct medical costs in the first year following a nonvertebral fracture in a managed care setting. Osteoporos Int 2006;17:252-258.



23. Qu B, Ma Y, Yan M, et al. The economic burden of fracture patients with osteoporosis in western China. Osteoporos Int 2014;25:1853-1860.



24. Tamulaitiene M, Alekna V. Incidence and direct hospitalisation costs of hip fractures in Vilnius, capital of Lithuania, in 2010. BMC Public Health 2012;12:495




Fig. 1
Age-standard incidence (per100,000) of osteoporotic fracture in Korean over 50 years old between 2008 and 2011.
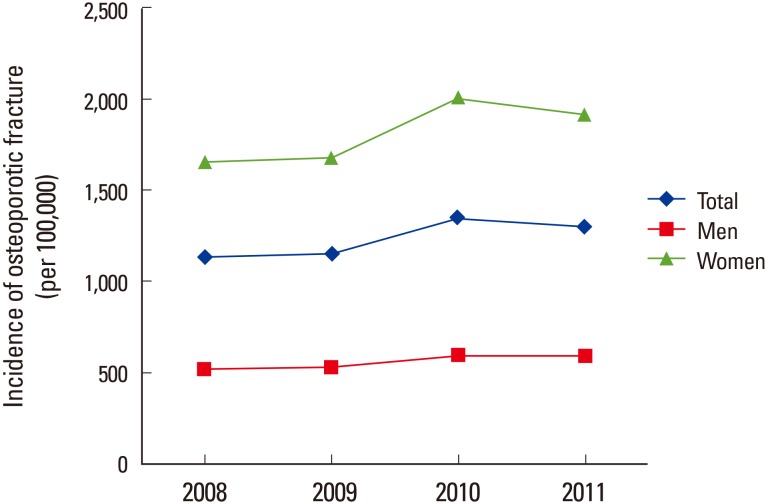
Fig. 2
Estimated cost according to healthcare resource for osteoporotic fracture. (A) Total health care cost ($, million) and (B) Mean health care cost ($).

Table 1
The absolute number of osteoporotic fracture after excluding patients with severe disease in Koreans over 50 years old

Table 2
Annual total healthcare costs ($, million) for osteoporotic fractures in Koreans over 50 years old between 2008 and 2011
- TOOLS
-
METRICS

-
- 52 Crossref
- 0
- 3,345 View
- 29 Download
- Related articles


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



