Health-related Quality of Life in Accordance with Fracture History and Comorbidities in Korean Patients with Osteoporosis
Article information
Abstract
Background
The purpose of this study was to explore health-related quality of life (HRQOL) among Korean patients with osteoporosis and to measure the impact of fractures and comorbidity on their quality of life (QOL) using the Korean National Health and Nutrition Examination Survey (KNHANES) data with a nationwide representativeness.
Methods
This study was based on 4-year-data obtained from the KNHANES 2008 to 2011. Osteoporosis was diagnosed in 2,078 survey participants according to their bone mineral density measurements using dual energy X-ray absorptiometry. According to the World Health Organization study group, T-scores at or above -1.0 are considered normal, those between -1.0 and -2.5 as osteopenia, and those at or below -2.5 as osteoporosis The EuroQol five-dimensional questionnaire (EQ-5D) index score was used to assess the QOL.
Results
Of 2,078 patients diagnosed with osteoporosis, fractures were found to occur at 11.02%. Wrist fracture was the most frequent, affecting 4.52% of the patients, with a significantly different prevalence among men and women (P<0.001). The overall EQ-5D index score was 0.84±0.01 among patients with osteoporosis. With the exception of cancer, the EQ-5D index score were significantly lower for those having osteoarthritis, rheumatoid arthritis, hypertension, diabetes, chronic obstructive pulmonary disease and cardiovascular events compared to those without the related diseases.
Conclusions
We found that low health utility was associated with previous spine fracture and comorbidities in patients with osteoporosis. In particular, the number of fracture experiences greatly deteriorated the HRQOL in patients with osteoporosis. Thus, prevention of secondary fractures and chronic care model for comorbidities should be a priority for osteoporosis management in order to improve HRQOL.
INTRODUCTION
Osteoporosis is one of common musculoskeletal diseases in elderly populations. Osteoporosis accompanied by osteoporotic fractures is notorious health problems and cause factors that degenerates quality of life (QOL) such as high mortality, decreased activity, and serious socioeconomic burden.[123] Although the mortality rate after osteoporotic fractures is either decreasing or maintaining a steady trend, residual disability after a fracture is still remains a major concern.[234]
Previous researches have focused on health-related QOL (HRQOL) in osteoporosis because increasing life expectancy and economic status among elderly populations cause them to divert their attention towards QOL, rather than mere survival.[56789101112] It was found that osteoporosis and osteoporotic fractures have a negative impact on HRQOL. However, reduction of QOL in osteoporotic fracture is depending on with type of fractures such as vertebrae, hip, wrist, and other anatomical sites, the characteristics of the study participants, and types of reported studies.[567891011121314151617]
In Korea, although researches on HQROL associated with various other diseases are available,[18192021] those related to osteoporosis and osteoporotic fractures are few.[1819] Therefore, we designed to explore HRQOL among Korean patients with osteoporosis and to measure the impact of fractures and comorbidity on their QOL using the Korean National Health and Nutrition Examination Survey (KNHANES) data with a nationwide representativeness.
METHODS
1. Participants
This study was based on data from the 2008 to 2011 KNHANES, which was conducted by the Korea Ministry of Health and Welfare. The KNHANES is a nationwide representative cross-sectional survey for the Korean population with a clustered, multistage, stratified, and rolling sampling design. It consists of three sections: a health interview, a health examination, and a dietary survey. The participant's general information on health is obtained through household interviews on health. First, we collected data of 9,473 participants from July 2008 through May 2011 who were eligible to the bone mineral density (BMD) screening. The BMD screening was exerted only on men 50 years of age or older and women with menopause during 2008 to 2011. Among them, 2,078 patients who were diagnosed with osteoporosis were selected for this study.
2. Health examination survey
A health questionnaire was used to obtain information on age, gender, education level, insurance type, smoking status (current, ex-smoker, non-smoker), alcohol intake (heavy drinker, drinker, non-drinker), and walking days per week (yes or no). In terms of health behaviors, walking activities were represented as walking days per week. Heavy drinking was defined as having 5 or more drinks in one sitting in a day for 5 or more days in the past 30 days.[20] Body weight and height were measured in light clothing with no shoes, and body mass index (BMI) was calculated as weight (kg) divided by height squared (m2). Information regarding comorbidities, including: osteoarthritis (OA), rheumatoid arthritis (RA), hypertension (HTN), diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), cardiovascular (CV) events as potential confounding factors were examined through the health interview survey. Here, COPD was determined when the forced expiratory volume in 1 second (FEV1) divided by forced vital capacity was less than 0.7.[21]
3. Measurement of BMD and diagnosis for osteoporosis
BMD (g/cm2) at the lumbar spine, femoral neck, and total proximal femur were measured by dual energy X-ray absorptiometry (DXA; Hologic Inc., Bedford, MA, USA). According to the WHO study group, the diagnosis of osteoporosis is based on T-score thresholds. T-scores at or above -1.0 are considered normal, those between -1.0 and -2.5 as osteopenia, and those at or below -2.5 as osteoporosis.[22]
4. Fracture detection in personal histories
Fracture events were recorded using a standardized self-administered questionnaire. Fractures clearly caused by high-trauma events were excluded. High-trauma events included motor vehicle accidents, violence, and falls from more than the standing height of the individual. We included fracture events at only six sites (vertebra, hip, wrist, humerus, clavicle, and ribs). In addition, historical height loss, which was calculated as the difference between the subject's current measured height and self-reported recalled tallest height, of 4.0 cm or more was regarded as indicative of a prevalent vertebral fracture.[232425]
5. HRQOL measures
HRQOL was evaluated using the EuroQol five-dimensional (EQ-5D) questionnaire, which generates assessment scores across five dimensions of health, namely, mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.Responses in each dimension were divided into three categories; no problem, moderate problem, or extreme problem. Average scores of the EQ-5D index were calculated to assess HRQOL, which is a preference-based health status index.[262728]
HRQOL should be interpreted with caution because HRQOL has socially and culturally dependent characteristics.[29] Since the preference weights of Koreans are quite different from those of Caucasians, we used Korean specific preference weight to generate EQ-5D index scores.[28] Average scores of the EQ-5D index ranged from -0.17 to 1, where 1 indicates no problem in any of the five dimensions, zero indicates death, and negative values indicate health statuses worse than death. In addition, respondents assessed their health statuses using a visual analogue scale (VAS), which ranged from 0 (worst imaginable health state) to 100 (best imaginable health state).[30]
6. Statistical analysis
The average value of the EQ-5D index was calculated to investigate the QOL among patients with osteoporosis by using a South Korean specific tariff based on the time-trade-off method.[28] The types of fractures experienced, number of fractures were considered in the calculation of the EQ-5D index score in order to examine how seriously fracture experiences (e.g. lesion of fractures, number of fractures) could affect their QOL. Also we considered comorbidity as one of critical factors contributing to the QOL. Given the age of prevalent population of osteoporosis, this study considered HTN, DM, depressive disorder, cancer, RA, OA, and CV events such as stroke, myocardial infarction and angina, and COPD as comorbidity. Statistical differences were tested with t-test or Chi-square (χ2) using PROC SURVEYFREQ or PROC SURVEYMEANS. SAS version 9.4 (SAS Inc., Cary, NC, USA) was used for analysis.
7. Ethics statement
This study's protocol for performing an analysis of the 2008 to 2011 KNHANES data was reviewed and approved by the Institutional Review Board (Approval No. 2008–04 EXP-01-C, 2009–01CON-03-C, 2010–02CON-21-C, and 2011–02CON-06-C) of the Korea Centers for Disease Control and Prevention (KCDC). Informed consent was obtained from all of the participants when the 2008, 2009, 2010, and 2011 KNHANES were conducted. All of the data were downloaded from the official website of the KNHANES (http://knhanes.cdc.go.kr/). These data are open to the public after completion of a designated registration process for access.
RESULTS
1. Population characteristics
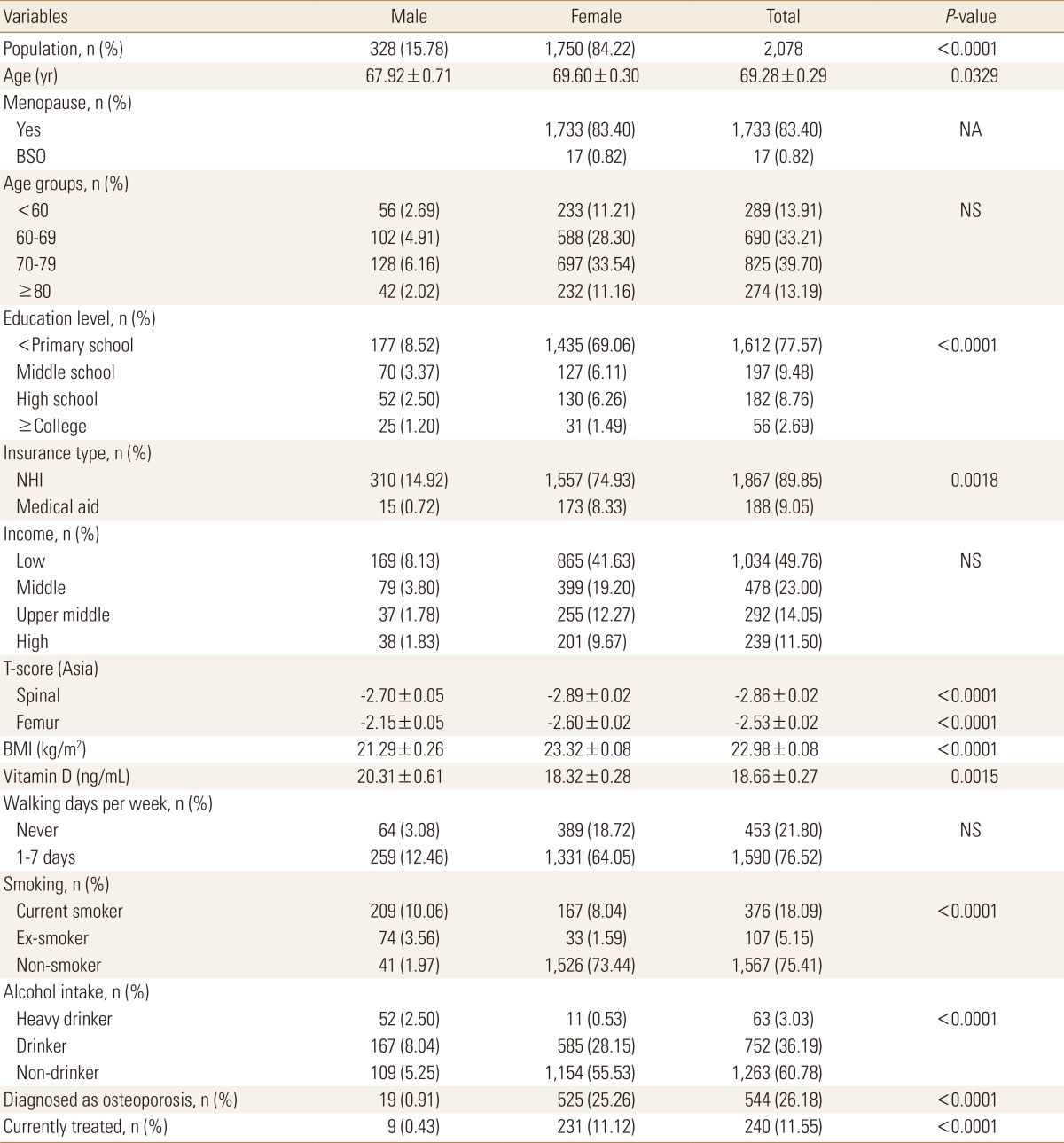
A total of 2,078 osteoporosis patients (328 men and 1,750 women) who had their T-scores at or below -2.5 were selected. Table 1 shows the general characteristics of these patients. Eighty-four percent of the study population were women with an average age of 69.60±0.30 years. Among them, 99.0% were naturally menopaused. Education level (P<0.0001) and insurance type (P=0.0018) revealed significant differences between men and women. T-scores in spine (-2.70 vs. -2.89) and femur (-2.15 vs. -2.60) were significantly lower in women than in men. BMI calculated as weight (kg) divided by height squared (m2) showed a significant difference between men and women (P<0.0001). Vitamin D level was significantly lower in women (P=0.0015). Walking activities did not differ between men and women while smoking habits and alcohol consumptions did differ significantly between men and women (P<0.0001).
The salient points were the rate of previous diagnoses with osteoporosis was only 26.18% (544/2,078) among the osteoporosis population, and the current treatment rate was 44.12% (240/544) among those already diagnosed.
2. Incidence of previous fractures
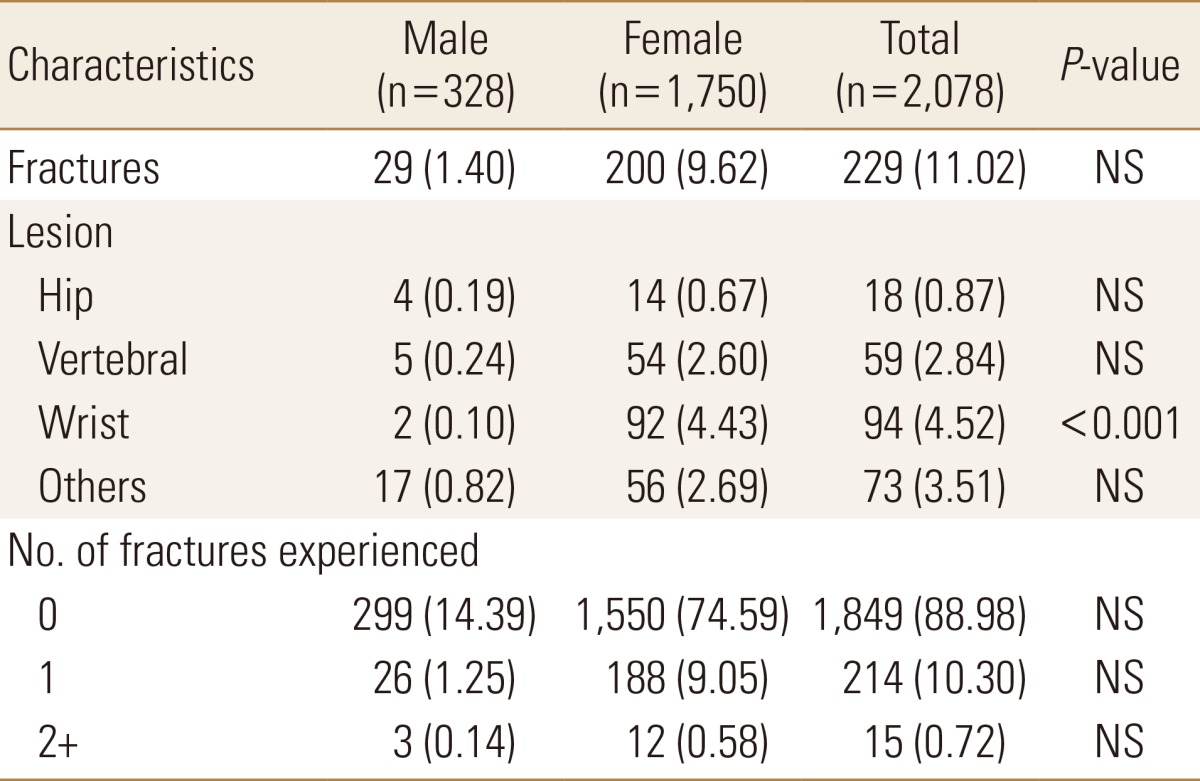
Fractures among osteoporosis patients were found to occur at 11.02%. Wrist fracture was the most frequent, at 4.52%, with a significantly different incidence among men and women (P<0.001). Next, spine fracture showed a incidence of 2.84%, followed by hip fracture at 0.87% (Table 2).
A majority of the osteoporosis patients (88.98%) reported that they had no fractures. It was found that 10.30% of the study population had fractures once, and 0.72% reported that they had experienced fractures twice or more.
3. EQ-5D scores in osteoporosis
The overall EQ-5D index score was 0.84±0.01 among patients with osteoporosis. Compared to the score of general population (0.95±0.001), this value showed lower QOL among osteoporosis patients. Men scored higher in the EQ-5D score than women (0.87 vs. 0.83 respectively, P=0.0033).
Their QOL may differ when it is accompanied by fractures and comorbidities including OA, HTN, DM, COPD, and CV events.
Figure 1 showed the scores of EQ-5D of those who had osteoporotic fractures or comorbidity compared with those of general population and patients with osteoporosis. As subgrouping osteoporosis patients by lesion of fractures and whether or not having comorbidities, EQ-5D scores were calculated. It can be inferred that having twice or more fractures mostly deteriorated the QOL according to Figure 1A.
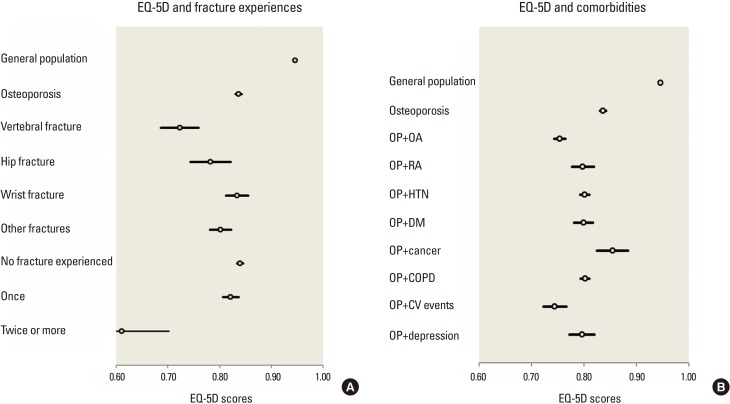
Health-related quality of life scores in accordance with fracture history and comorbidity. (A) EuroQol five-dimensional questionnaire (EQ-5D) and fracture sites. (B) EQ-5D and comorbidities. OP, osteoporosis; OA, osteoarthritis; RA, rheumatoid arthritis; HTN, hypertension; DM, diabetes mellitus; COPD, chronic obstructive pulmonary disease; CV events, cardiovascular events.
When it comes to comorbidity, OA and CV events showed greatly lowered scores of HRQOL while cancer did not have significantly lower scores.
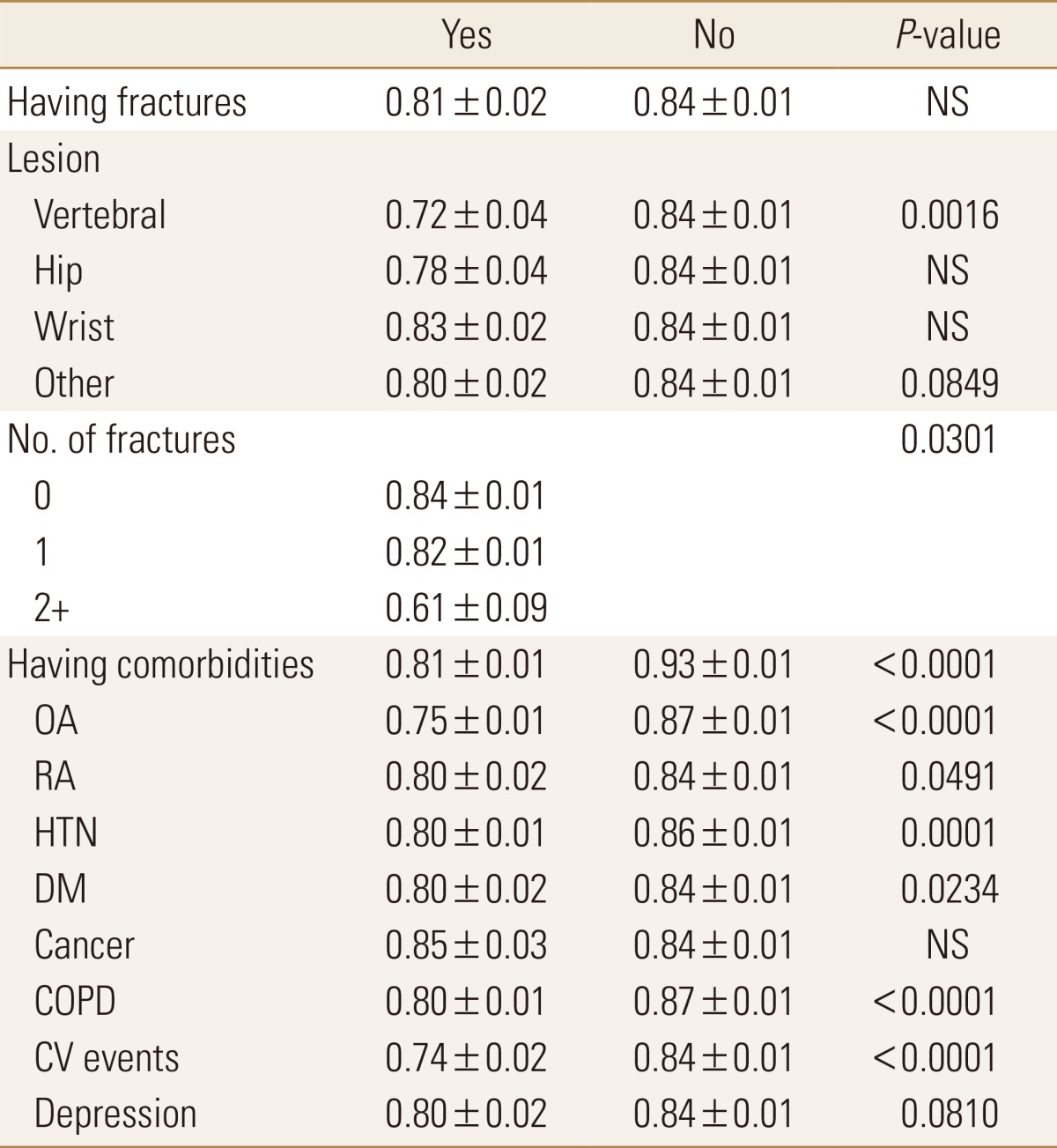
Table 3 shows the EQ-5D index scores at each osteoporotic health state with statistical significances. Patients with fracture experiences showed lower EQ-5D scores (0.81±0.02) than those with no fractures (0.84±0.01). However, only vertebral fractures showed a significantly lower QOL score (0.72±0.04) than having no vertebral fractures (0.84±0.01; P=0.0016).
Un-adjusted EuroQol five-dimensional questionnaire scores in accordance with fracture aspects and comorbidities
Hip fractures negatively impacted on the QOL among osteoporosis patients but with no significant difference (0.78±0.04 vs. 0.84±0.01). Other fractures had a marginal significance (P=0.0849).
HRQOL among patients with comorbidities (Fig. 1B and Table 3) were negatively impacted than HRQOL among those without comorbidities (P<0.0001). With the exception of cancer, the EQ-5D index score were significantly lower for those having OA (0.75±0.01), RA (0.80±0.02), HTN (0.80±0.01), DM (0.80±0.02), COPD (0.80±0.01), and CV events (0.74±0.02) compared to those without the related diseases. Depression demonstrated a lower value in the EQ-5D compared to having no depression (P=0.081).
DISCUSSION
This study examined HRQOL among patients with osteoporosis and osteoporotic fractures using nationwide survey data in South Korea. Our results demonstrated that having vertebral fractures, number of fractures experienced negatively affected HRQOL of osteoporosis patients.
The decrease of QOL is depending on the characteristics of the study participants, types of reported studies, number of fractures, and the type of fractures.[567891011121314151617] Many studies reported a negative relationship between HRQOL and osteoporotic fracture. Several studies reported that a history of fracture was affecting the health status of postmenopausal women.[73132] Hagino et al.[9] performed a prospective observational study for sequential change during one year in QOL for patients with osteoporotic fractures including hip, spine, and wrist. The decrease in HRQOL was the most serious in patients with hip fractures followed by spine fractures. However, HRQOL in patients with wrist fractures recovered back to nearly preinjury status 6 months after the injury.
Although vertebral fracture had impacted the HRQOL scores, having fracture experiences twice or more was found to have greatly deteriorated the EQ-5D scores in this study. This implies that the prevention of secondary fractures is crucial to maintaining the QOL among osteoporosis patients.[ 133233]
Some studies reported the importance of comorbidity in its effects on HRQOL in patients with osteoporosis.[313435363738] Bianchi et al.[31] performed a case-control study and reported that chronic diseases such as pain and depressed mood were negatively correlated with HRQOL in osteoporotic women. Salaffi et al.[37] performed an evaluation of effect of HRQOL in patients with osteoporosis using 234 women with vertebral fractures and 244 asymptomatic women. They reported that comorbidities (the simultaneous presence of one or more health conditions in a patient with a defined index condition) was an important contributor to the reduced HRQOL. Guillemin et al.[38] performed HRQOL among 7,897 European and United States women with osteoporosis in a large international study. They reported that young age, low BMI, previous vertebral fracture, increased number of comorbidities, high fear of falling and depression were associated with reduced HRQOL. These findings correspond with our study. We found that osteoporotic fractures and comorbidity such as CV events, RA, OA and COPD were associated with reduced HRQOL.
This study has several limitations. The incidence of fractures relied on patients' reports without verification using radiographic findings. However, in our experience, most patients who experienced fractures tended to remember their history of fractures. However, our study will be informative for health professionals and decision makers.
In conclusion, this study of HRQOL using nationwide survey database provides evidence that a low health utility depends on whether or not having previous spine fracture or comorbidities in patients with osteoporosis. Above all, the number of fracture experiences greatly deteriorated the HRQOL in patients with osteoporosis. Thus, prevention of secondary fractures and chronic care model for comorbidities should be a priority for osteoporosis management in order to improve QOL.
Notes
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HC15C1189).
No potential conflict of interest relevant to this article was reported.