 |
 |
| jbm > Volume 28(3); 2021 > Article |
|
Abstract
Background
Methods
Acknowledgments
DECLARATIONS
Funding
The specific collagen peptides (product name FORTIBONE®) were provided by the GELITA GmbH, Eberbach Germany.
Ethics approval and consent to participate
The original interventional study (DRKS00009708) was conducted according to the guidelines of the Declaration of Helsinki, and approved by the independent Ethics Committee of the University of Freiburg.
Authors’ contributions
Conceptualization: DZ, SO, and DK; Data curation: DZ and DK; Formal analysis: DZ and DK; Writing-original draft preparation: DZ, SO, and DK; Writing-review and editing: DZ, SO, and DK; All authors read and approved the final manuscript.
Conflict of interest
No potential conflict of interest relevant to this article was reported. SO has given scientific lectures that were in parts supported by the GELITA AG. He is also co-inventor of patents concerning the use of collagen peptides. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results. The authors responsible for data assessment and analysis have neither financial nor competing interests concerning the outcome of this investigation.
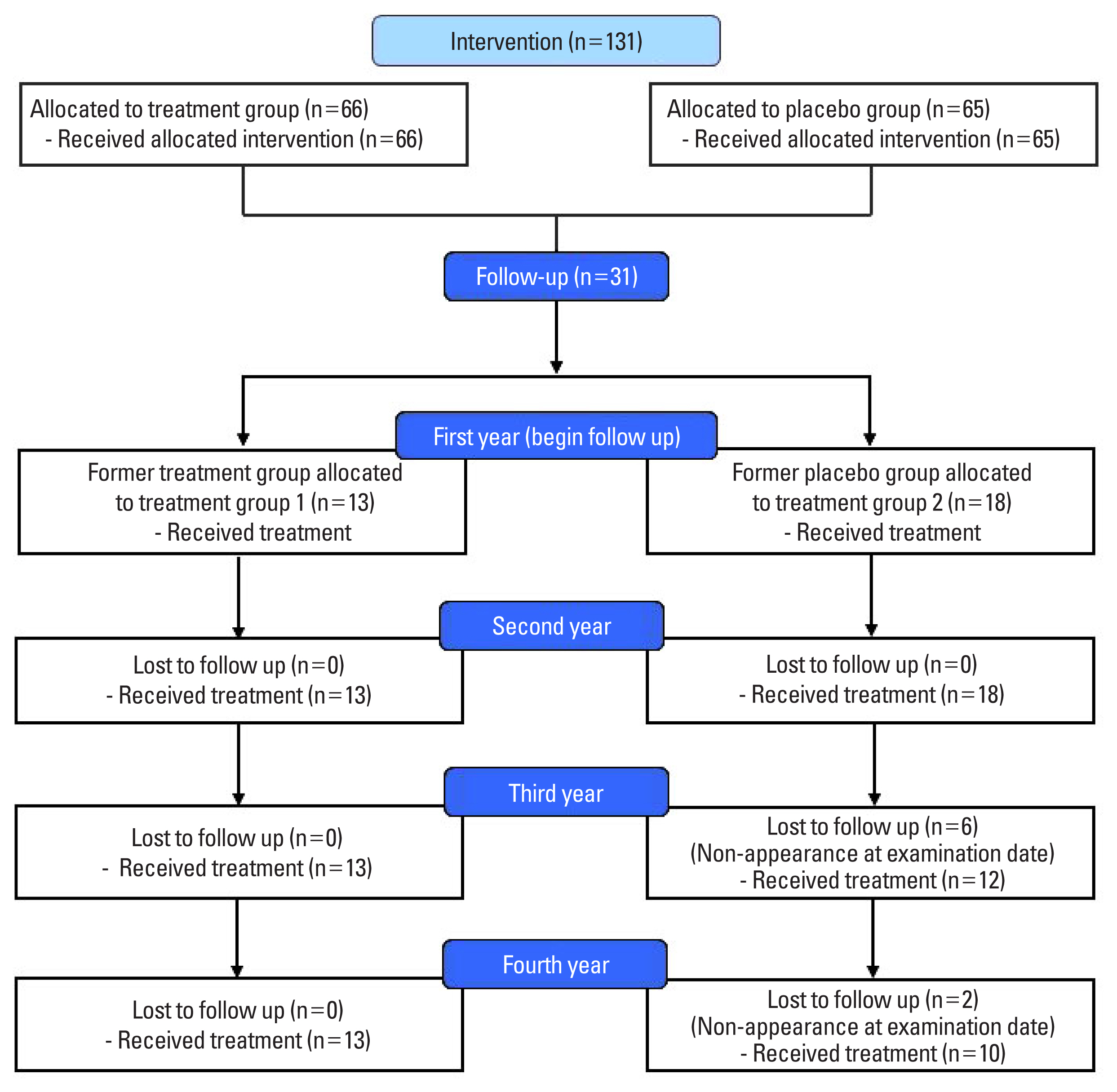
Fig. 2

Table 1
| Total (N=31) | Group 1 (N=13) | Group 2 (N=18) | P-valuea) | |
|---|---|---|---|---|
| Age (yr) | 62.9±7.21 | 62.9±8.57 | 62.9±6.31 | 0.987 |
| Height (m) | 1.62±0.067 | 1.62±0.061 | 1.61±0.072 | 0.505 |
| Body weight (kg) | 61.4±9.42 | 63.2±9.93 | 60.2±9.11 | 0.387 |
| BMI (kg/m2) | 23.6±4.10 | 23.8±3.51 | 23.4±4.57 | 0.773 |
| RRsyst (mmHg) | 123.4±27.5 | 115.5±30.6 | 128.6±24.7 | 0.208 |
| RRdia (mmHg) | 82.7±11.0 | 79.2±9.00 | 85.0±11.8 | 0.157 |
| BMD spine (g·cm−2) | 0.778±0.095 | 0.773±0.108 | 0.783±0.086 | 0.784 |
| BMD femur (g·cm−2) | 0.796±0.085 | 0.815±0.101 | 0.782±0.072 | 0.307 |
| T-score spine | −2.47±0.823 | −2.52±0.943 | −2.44±0.751 | 0.784 |
| T-score femur | −1.43±0.689 | −1.28±0.813 | −1.54±0.583 | 0.304 |
REFERENCES
- TOOLS
-
METRICS

- ORCID iDs
-
Denise Zdzieblik

https://orcid.org/0000-0001-8637-8757Daniel König

https://orcid.org/0000-0001-7002-1286 - Related articles


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



