INTRODUCTION
METHODS
1. Do you prescribe BTMs when you prescribe AOMs to your patients with osteoporosis?
2. If you prescribe BTMs, what kinds of them do you prescribe? (Multiple responses are available)
- serum osteocalcin
- serum bone specific alkaline phosphatase (sBSALP)
- serum carboxyl-terminal propeptide of type I collagen
- serum amino-terminal propeptide of type I collagen (sP1NP)
- serum C-terminal telopeptide of type I collagen (CTX-I)
- urine CTX
- serum N-terminal telopeptide of collagen type I (sNTX-1)
- urine NTX
- urine free and total pyridinoline
- urine free and total deoxypyridinoline (uDPD)
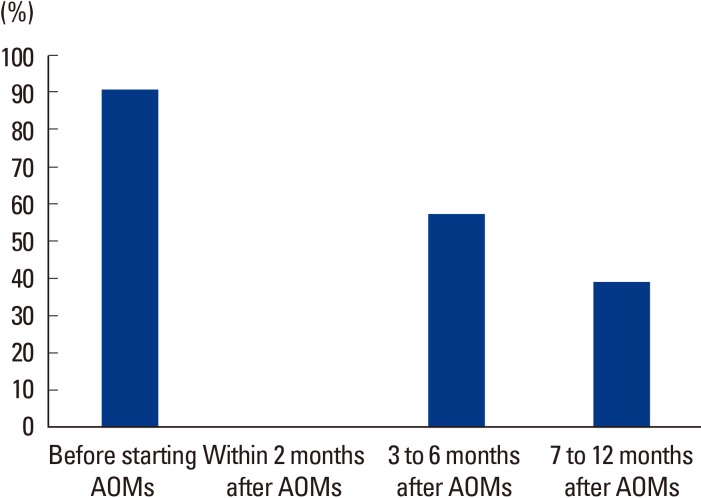
3. If you prescribe BTMs, when do you prescribe them? (Multiple responses are available)
- before starting AOMs
- within 2 months after starting AOMs
- between 3 and 6 months after starting AOMs
- between 7 and 12 months after starting AOMs
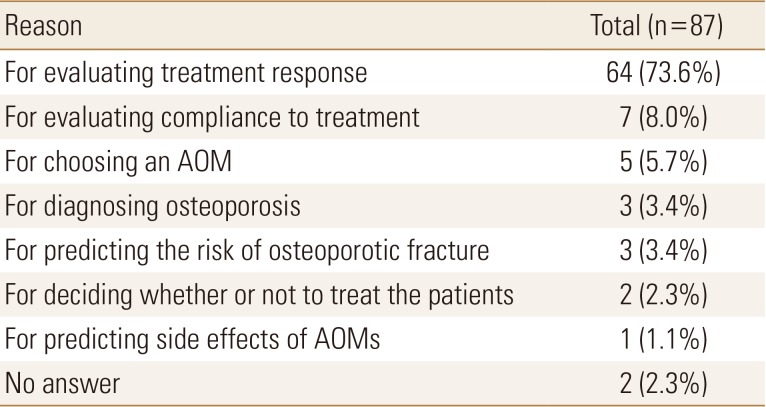
4. If you prescribe BTMs, what purpose do you prescribe them for?
- for diagnosing osteoporosis
- for predicting the risk of osteoporotic fracture
- for choosing an AOMs
- for evaluating treatment response
- for evaluating compliance to treatment
- for predicting side effects of AOMs
- for deciding whether or not to treat the patients
5. If you prescribe BTMs, how do you evaluate the efficacy or compliance of AOMs (anti-resorptive drugs)?
- percent change of BTMs
- change of absolute values of BTMs
- if the value of BTMs reach the target
6. If you prescribe BTMs, what is the difficulty in the prescription of them?
- proper choice of BTMs
- interpretation of BTMs results
- proper sampling of BTMs
- no difficulty
7. If you do not prescribe BTMs, what is the reason?
- It is impossible to prescribe BTMs in our medical center.
- I do not feel the necessity of BTMs, although it is possible to prescribe them in our medical center.
- I have no idea which BTMs to be prescribed, although I feel the necessity of them and it is possible to prescribe these markers in our medical center.
8. What do you think to be supplemented in the clinical utility of BTMs in Korea?




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






