 |
 |
| jbm > Volume 31(1); 2024 > Article |
|
Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic and the consequent social distancing period are thought to have influenced the incidence of osteoporotic fracture in various ways, but the exact changes have not yet been well elucidated. The purpose of this study was to investigate the impact of the COVID-19 pandemic on the incidence of osteoporotic fracture using a nationwide cohort.
Methods
The monthly incidence rates of vertebral; hip; and non-vertebral, non-hip fractures were collected from a nationwide database of the Korean National Health Insurance Review and Assessment from July 2016 to June 2021. Segmented regression models were used to assess the change in levels and trends in the monthly incidence of osteoporotic fractures.
Results
There was a step decrease in the incidence of vertebral fractures for both males (6.181 per 100,000, P=0.002) and females (19.299 per 100,000, P=0.006). However, there was a negative trend in the incidence of hip fracture among both males (−0.023 per 100,000 per month, P=0.023) and females (−0.032 per 100,000 per month, P=0.019). No impact of COVID-19-related social distancing was noted.
Coronavirus disease 2019 (COVID-19) is a respiratory pandemic caused by a new coronavirus known as severe acute respiratory syndrome coronavirus 2. It began spreading rapidly in December 2019.[1] South Korea was once the second most affected country after China in early 2020, following a massive outbreak of COVID-19 that occurred in the Daegu region.[2] As of June 30, 2021, a total of 156,961 confirmed cases had been reported in South Korea. This pandemic has induced significant strain on the healthcare system.[3]
In February 2020, South Korea implemented social distancing measures to contain the spread of the disease and reduce the burden on healthcare resources.[4] Data on the incidence of osteoporotic fractures during COVID-19 are conflicting, with some studies showing that the incidence of fractures remained stable [5-8] while many others indicate a reduction.[7,9-12] Possible causes include mobility restrictions, changes in public behavior, and the allocation of medical resources and manpower.
Given the high heterogeneity in the behavior of osteoporotic fractures during COVID-19 so far, there is a need to study the local patterns and compare them to data from previous years. The incidence of hip fractures in South Korea is known to remain stable, but the incidence of vertebral fractures or fractures at other sites has not been studied thus far.[8]
The objective of this study is to describe the impact of the COVID-19 pandemic on the incidence of osteoporotic fractures in South Korea.
This retrospective nationwide study identified subjects from the Korean National Health Insurance Review and Assessment Service (HIRA) database from July 2016 to June 2021 (Fig. 1). We identified subjects aged 50 years and older at the time of osteoporotic fracture. Osteoporotic fracture events were defined using inpatient diagnoses with the International Classification of Diseases (ICD), Ninth/Tenth revision codes and procedural codes based on previous studies.
The operational definitions of osteoporotic fractures of vertebra, hip, humerus, and distal radius were made using ICD-10 codes and procedure codes using the National Health Insurance Service data. ICD-10 codes for vertebral fracture were; S22.0 (fracture of the thoracic spine), S22.1 (multiple fractures of the thoracic spine), S32.0 (fracture of the lumbar spine), S32.7 (multiple fractures of the lumbar spine), T08.0 (fracture of the spine), M48.4 (fatigue fracture of vertebra), M48.5 (collapsed vertebra), M49.5 (collapsed vertebra), and M80.8 (other osteoporosis with pathological fracture). ICD codes of hip fractures were S72.0 (fracture of the femur neck) and S72.1 (trochanteric fracture). ICD-10 codes of humerus fractures were S42.2 (fracture of upper end of humerus), S42.3 (fractured shaft of humerus), and codes for distal radius fractures were S52.5 (fracture of lower end of radius) and S52.6 (fracture of lower end of both ulnar and radius).[13,14] Details about our operational definitions are provided in supplements (Supplementary Table 1).
We summarized the patients’ demographic characteristics (age group, and sex) and index year. Categorical variables were expressed as numbers and percentages. Monthly incidence rate (IR) of vertebral, hip, non-vertebral, non-hip (NVNH) fractures were presented as the number of newly diagnosed fractures in a month per 100,000 person-years from September 2016 to May 2021.[15]
Changes in levels and trends in the monthly IR of each fracture the before and after the COVID-lockdown (January 2020) were estimated using segmented regression models. The models were tested for autocorrelation using the Durbin-Watson statistics.[16] Since baseline IR differed between sex and age group, we assessed the changes in levels and trends in the monthly incidence for sex and age group separately. All P-values less than 0.05 were considered statistically significant. Statistical analyses were performed using SAS EG statistical software version 7.1 (SAS Institute, Cary, NC, USA).
From July 2016 to June 2021, there were 18,004,216 cases of osteoporotic fractures in patients aged 50 years and older (Fig. 1). Among these, 9,038,250 cases were diagnosed with vertebral fractures, and 1,781,218 incident patients were included from January 2017 to May 2021. Additionally, 2,456,247 cases were diagnosed with hip fractures, with 168,578 incident patients were included. 6,509,719 cases were diagnosed with NVNH fractures, and 593,386 incident patients were included, making vertebral fractures the most frequently reported osteoporotic fracture.
Table 1 presents the clinical characteristics of study subjects. Females were more common than males in all fracture groups (76.8% in vertebral fractures, 72.3% in hip fractures, 80.5% in NVNH fractures). Vertebral fractures were most prevalent in the 70 to 79 age group (38.4%), while hip fractures were most common in the 80+ age group (53.7%).
The IRs of osteoporotic fractures are presented in Figure 2. A notable decrease in vertebral fractures among females was observed during the social distancing period, while a mild dip was noted in vertebral fracture among males. The decline was greatest in the 70 to 79 age group and the 80+ age group.
There was a seasonality in hip fractures with a peak every winter. The peak decreased over time, showing a negative trend for both male and female. There was no difference in pattern within the social distancing period. A similar pattern was found for NVNH fractures with seasonality but no difference within the social distancing period.
Segmented regression analysis with autoregression was done to evaluate the impact of COVID-19 social distancing period on osteoporotic fracture incidence (Fig. 3, Table 2). A step decrease was noted in vertebral fracture for both male (6.181 per 100,000, P=0.002) and female (19.299 per 100,000, P=0.006). There was no time trend in vertebral fractures. In subgroup analysis by age, the step decrease was statistically significant in the 70 to 79 age group and 80+ age group, but not in 50 to 59 age group and 60 to 69 group (Supplementary Table 2).
There was a negative trend in hip fracture among both male (−0.023 per 100,000 per month, P=0.023) and female (−0.032 per 100,000 per month, P=0.019). No impact of COVID-19 social distancing period was noted. Negative trend was also found for NVNH fractures among both male (−0.095 per 100,000 per month, P<0.001) and female (−0.489 per 100,000 per month, P=0.004). Subgroup analysis by age revealed a step decrease of vertebral fractures among 70 to 79 females (−1.786 per 100,000, P=0.022). In nearly all fracture and age groups except for vertebral fractures among 70 to 79 females, there was a consistent negative trend and no impact of COVID-19 social distancing (Supplementary Table 3, 4).
In this study, we found a step decrease in vertebral fractures during the COVID-19 social distancing period among adults in South Korea. Further, we observed a negative trend in hip fractures, which was not influenced by COVID-19 social distancing period.
The decline in vertebral fractures can be attributed to the limitation of mobility, since social distancing has led to a reduction of public movement and outdoor activities.[17] The decrease in vertebral fractures may also be partly attributed to a decrease in detection due to decreased healthcare use and imaging study. It is well known that the number of emergency department visits has decreased worldwide since the onset of the COVID-19 pandemic.[18,19] However, considering that the decrease in healthcare use is mainly non-orthopedic and that orthopedic admissions display a relatively minor change, it is reasonable to infer that mobility restrictions have contributed to the reduction in vertebral fractures.[20]
It is interesting to note that the incidence of hip fractures did not decrease within the COVID-19 social distancing period, in contrast to the incidence of vertebral fractures. Our findings are consistent with those of previous studies reporting that the incidence of hip fractures and low-energy trauma did not decrease during the COVID-19 pandemic.[21-23] The reason for the difference in these patterns is not fully understood.
Age-adjusted hip fracture rates worldwide show differences in the trends and their timing between countries and continents, with some countries showing a plateau or beginning to decline in hip fractures rates, while others continue to increase.[21,24] In South Korea, the incidence of hip fracture is known to increase rapidly until 2012 from a nationwide database.[25] However, our study found that there is a negative trend in hip fracture incidence, suggesting that the decline may have begun, as in other countries such as the USA or Taiwan.[26,27] The etiologies of the secular patterns are not fully understood and declared factors include urbanization, birth cohort effects, changes in bone mineral density and body mass index, osteoporosis medication use, and/or lifestyle interventions, such as smoking cessation, improvement in nutritional status, and fall prevention.[24] Further studies are needed to confirm the change in the secular trend and to clarify the etiology.
Our study has several limitations. First, the data we collected did not include a lifetime history of previous fractures and a diagnosis of osteoporosis. Considering baseline fracture risk based on these histories would be useful for analyzing the true fracture trend and IR in future studies. Second, this study was a retrospective observational study using a national health insurance claims database, and there was a possibility of misclassification in defining study subjects. However, we made efforts to adopt a valid operational definition, incorporating diagnostic codes, procedure codes, and hospital admissions. A recent study comparing diagnoses from claims databases with medical records showed overall positive predictive value rates ranging from 59.7% to 98.2% for osteoporotic fractures at various sites.[28-30] Thus, we believe that misclassification of study outcomes might be low and would not significantly affect the main results. Third, due to the nature of this study using a national health insurance claims database, only clinical fractures were detected, and morphometric fractures were not included. Fourth, the incidence of osteoporotic fractures described in this study might be overestimated due to subsequent fracture within the same year, as we summed up monthly incidences of osteoporotic fractures rather than calculating yearly incidence. It is important to note that the objective of this study is to determine the trend and impact of COVID-19, not to provide epidemiological data, and should be interpreted accordingly. Lastly, our data were limited to June 2021, and we were unable to describe the trend after COVID-19. Further studies are needed to determine whether the changes found in this study will return to their original state after COVID-19.
In conclusion, during the early days of the COVID-19 pandemic, vertebral fracture incidence considerably decreased with the implementation of government social distancing measures.
Acknowledgments
The authors would like to thank the Health Insurance Review & Assessment (HIRA) Service of Korea for sharing invaluable national health insurance claims data in a prompt manner for this study (Project number: M20220103754).
DECLARATIONS
Funding
This study was supported by research funding from Korean Society for Bone and Mineral Research (Namki Hong, 2018).
Fig. 2
(A) Incidence rates of osteoporotic fracture. Monthly incidence rates of osteoporotic fractures are shown according to sex (B, C), location of fracture (D-F), and age (G-I). M, male; F, female; NVNH, non-vertebral, non-hip.
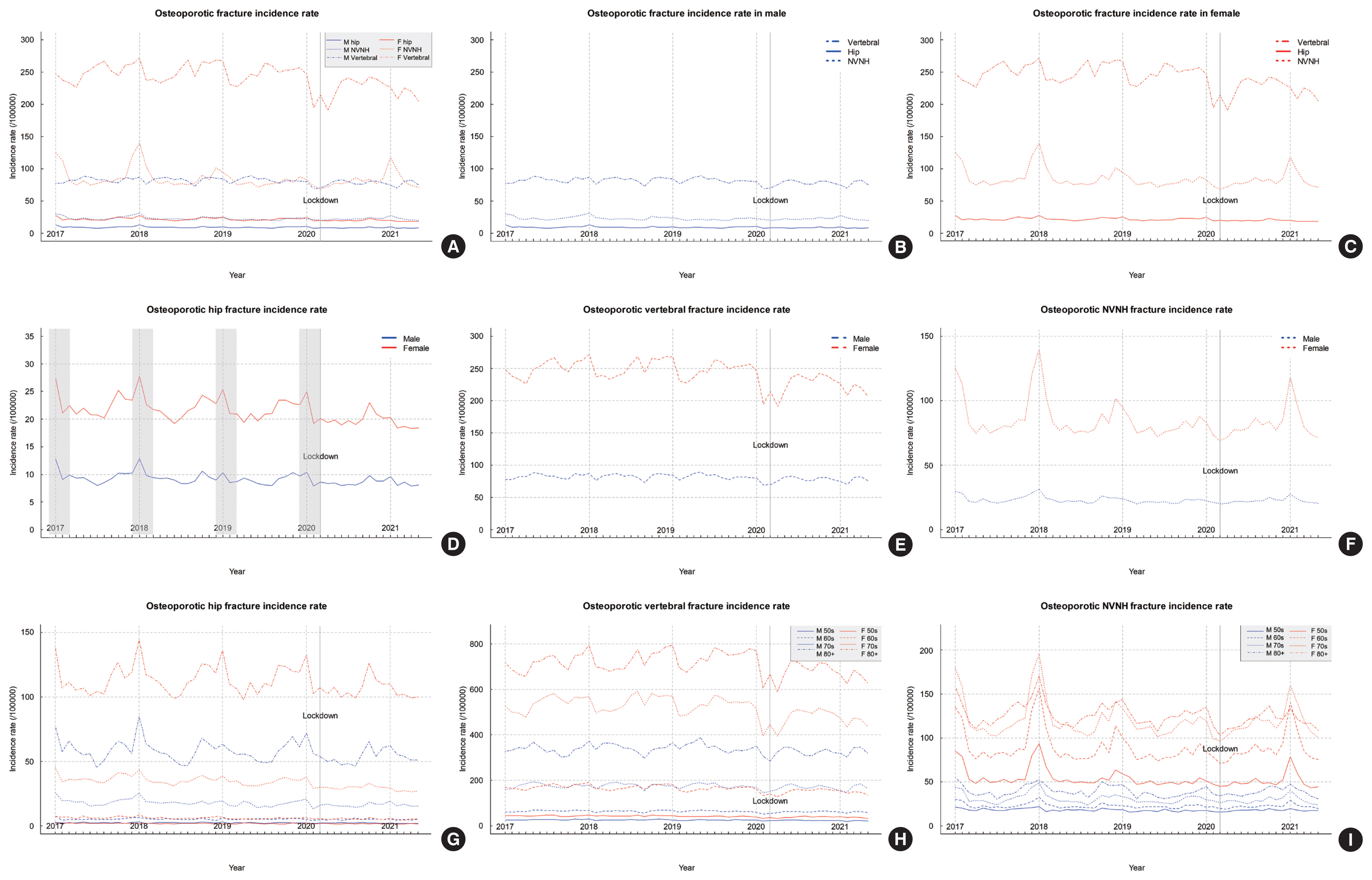
Fig. 3
(A-C) Segmented regression analysis for monthly incidence rates of osteoporotic fractures. Analysis was done according to location of fracture. M, male; F, female; NVNH, non-vertebral, non-hip.

Table 1
Baseline characteristics of study subjects
Table 2
Parameter estimates, standard error and P-values from the full segmented regression models predicting monthly osteoporotic fracture incidence in South Korea from January 2017 to May 2021
REFERENCES
1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 2020;382:727-33.
https://doi.org/10.1056/NEJMoa2001017.



2. Jang JG, Hur J, Choi EY, et al. Prognostic factors for severe coronavirus disease 2019 in Daegu, Korea. J Korean Med Sci 2020;35:e209.
https://doi.org/10.3346/jkms.2020.35.e209.



3. Miranda I, Ferrás-Tarragó J, Colado J, et al. Impact of the COVID-19 pandemic and the strict population confinement on hip fracture incidence in Spain: a systematic review. Rev Esp Geriatr Gerontol 2023;58:101380.
https://doi.org/10.1016/j.regg.2023.101380.



4. Choe YJ, Lee JK. The impact of social distancing on the transmission of influenza virus, South Korea, 2020. Osong Public Health Res Perspect 2020;11:91-2.
https://doi.org/10.24171/j.phrp.2020.11.3.07.



5. Nuñez JH, Sallent A, Lakhani K, et al. Impact of the COVID-19 pandemic on an emergency traumatology service: experience at a tertiary trauma centre in Spain. Injury 2020;51:1414-8.
https://doi.org/10.1016/j.injury.2020.05.016.



6. Chung JW, Ha YC, Lee MK, et al. Hip fracture management during the COVID-19 pandemic in South Korea. Clin Orthop Surg 2021;13:474-81.
https://doi.org/10.4055/cios21123.



7. Hall AJ, Clement ND, MacLullich AMJ, et al. IMPACT of COVID-19 on hip fracture services: a global survey by the International Multicentre Project Auditing COVID-19 in Trauma & Orthopaedics. Surgeon 2022;20:237-40.
https://doi.org/10.1016/j.surge.2021.04.007.



8. Jang SY, Cha Y, Kim Y, et al. Analysis of the effects of COVID-19 on hip fractures in Korea without lockdown: interrupted time series analysis using a nationwide cohort. J Korean Med Sci 2023;38:e137.
https://doi.org/10.3346/jkms.2023.38.e137.



9. Luengo-Alonso G, Pérez-Tabernero FG, Tovar-Bazaga M, et al. Critical adjustments in a department of orthopaedics through the COVID-19 pandemic. Int Orthop 2020;44:1557-64.
https://doi.org/10.1007/s00264-020-04647-1.



10. Wong JSH, Fang CX, Lee ALH, et al. Fracture incidence and fracture-related mortality decreased with decreases in population mobility during the early days of the COVID-19 pandemic: an epidemiological study. Hong Kong Med J 2023;29:31-8.
https://doi.org/10.12809/hkmj209116.


11. Lopez Gavilanez E, Navarro Chávez M, Gavilanes AWD, et al. Decreasing incidence rates of osteoporotic hip fractures in Ecuador during the COVID-19 pandemic. Arch Osteoporos 2022;18:15.
https://doi.org/10.1007/s11657-022-01202-w.



12. Surís X, Vela E, Clèries M, et al. Effects of COVID-19 confinement on the incidence and mortality of major osteoporotic fractures: an observational study in Catalonia, Spain. Arch Osteoporos 2022;17:150.
https://doi.org/10.1007/s11657-022-01193-8.



13. Ahn SH, Park SM, Park SY, et al. Osteoporosis and osteoporotic fracture fact sheet in Korea. J Bone Metab 2020;27:281-90.
https://doi.org/10.11005/jbm.2020.27.4.281.



14. Park SM, Ahn SH, Kim HY, et al. Incidence and mortality of subsequent vertebral fractures: analysis of claims data of the Korea National Health Insurance Service from 2007 to 2016. Spine J 2020;20:225-33.
https://doi.org/10.1016/j.spinee.2019.09.025.


15. Statistics Korea. Statistics on national population 2023 [cited by 2023 Dec 1]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B04005N&conn_path=I2.
16. Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002;27:299-309.
https://doi.org/10.1046/j.1365-2710.2002.00430.x.


17. Park IN, Yum HK. Stepwise strategy of social distancing in Korea. J Korean Med Sci 2020;35:e264.
https://doi.org/10.3346/jkms.2020.35.e264.



18. Westgard BC, Morgan MW, Vazquez-Benitez G, et al. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med 2020;76:595-601.
https://doi.org/10.1016/j.annemergmed.2020.06.019.



19. Visser M, Schaap LA, Wijnhoven HAH. Self-reported impact of the COVID-19 pandemic on nutrition and physical activity behaviour in dutch older adults living independently. Nutrients 2020;12:3708.
https://doi.org/10.3390/nu12123708.



20. Nourazari S, Davis SR, Granovsky R, et al. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am J Emerg Med 2021;42:203-10.
https://doi.org/10.1016/j.ajem.2020.11.029.



21. Johansen A, Inman DS. A view of COVID-19 from the perspective of the national hip fracture database. Bone Joint J 2021;103B:1007-8.
https://doi.org/10.1302/0301-620x.103b6.Bjj-2021-0326.


22. Malik-Tabassum K, Robertson A, Tadros BJ, et al. The effect of the COVID-19 lockdown on the epidemiology of hip fractures in the elderly: a multicentre cohort study. Ann R Coll Surg Engl 2021;103:337-44.
https://doi.org/10.1308/rcsann.2020.7071.



23. Pluskiewicz W, Wilk R, Adamczyk P, et al. The incidence of arm, forearm, and hip osteoporotic fractures during early stage of COVID-19 pandemic. Osteoporos Int 2021;32:1595-9.
https://doi.org/10.1007/s00198-020-05811-4.



24. Ballane G, Cauley JA, Luckey MM, et al. Secular trends in hip fractures worldwide: opposing trends East versus West. J Bone Miner Res 2014;29:1745-55.
https://doi.org/10.1002/jbmr.2218.


25. Kim BS, Lim JY, Ha YC. Recent epidemiology of hip fractures in South Korea. Hip Pelvis 2020;32:119-24.
https://doi.org/10.5371/hp.2020.32.3.119.



26. Berry SD, Daiello LA, Lee Y, et al. Secular trends in the incidence of hip fracture among nursing home residents. J Bone Miner Res 2020;35:1668-75.
https://doi.org/10.1002/jbmr.4032.



27. Chen FP, Shyu YC, Fu TS, et al. Secular trends in incidence and recurrence rates of hip fracture: a nationwide population-based study. Osteoporos Int 2017;28:811-8.
https://doi.org/10.1007/s00198-016-3820-3.



28. Yu MH, Hong N, Lee S, et al. Operational definition identifying osteoporotic vertebral fractures in the claims database. J Korean Med Sci 2022;37:e249.
https://doi.org/10.3346/jkms.2022.37.e249.



29. Lee YK, Park C, Won S, et al. Validation of an operational definition to identify distal radius fractures in a national health insurance database. J Hand Surg Am 2021;46:1026e1-e7.
https://doi.org/10.1016/j.jhsa.2021.03.001.


30. Park C, Jang S, Jang S, et al. Identification and validation of osteoporotic hip fracture using the national health insurance database. J Korean Hip Soc 2010;22:305-11.
https://doi.org/10.5371/jkhs.2010.22.4.305.

- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,422 View
- 19 Download
- ORCID iDs
-
Seungjin Baek

https://orcid.org/0009-0006-9271-4802Ye-Jee Kim

https://orcid.org/0000-0002-3307-2970Beom-Jun Kim

https://orcid.org/0000-0001-8591-1759Namki Hong

https://orcid.org/0000-0002-8246-1956 - Related articles
-
The Impact of COVID-19 on the Optimal Management of Osteoporosis2021 May;28(2)
Factors Affecting Bone Mineral Density Measurement after Fracture in South Korea2017 November;24(4)




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement1
Supplement1 Print
Print



