Position Statement: Atypical Femoral Fracture from the Korean Society for Bone and Mineral Research in 2023
Article information
Abstract
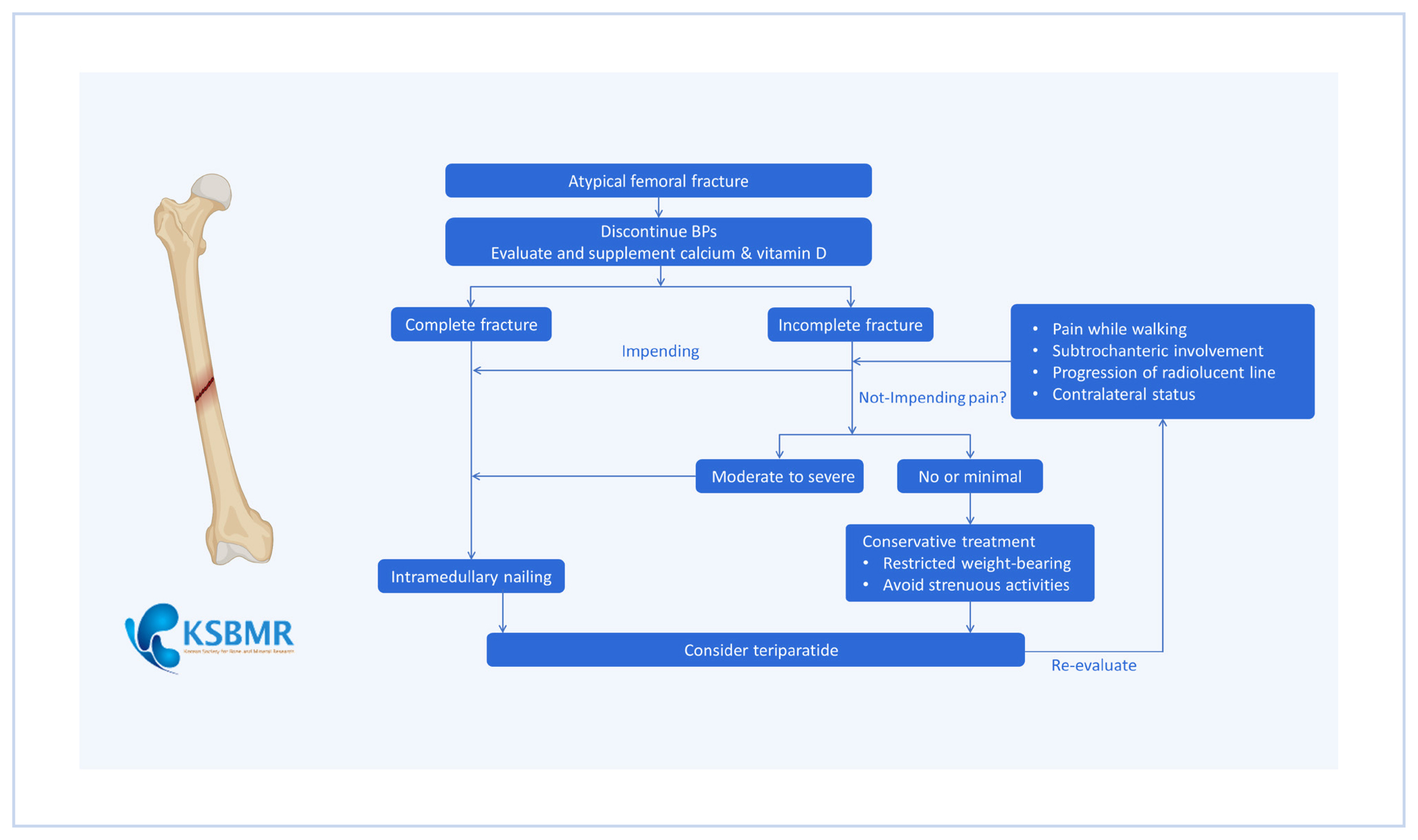
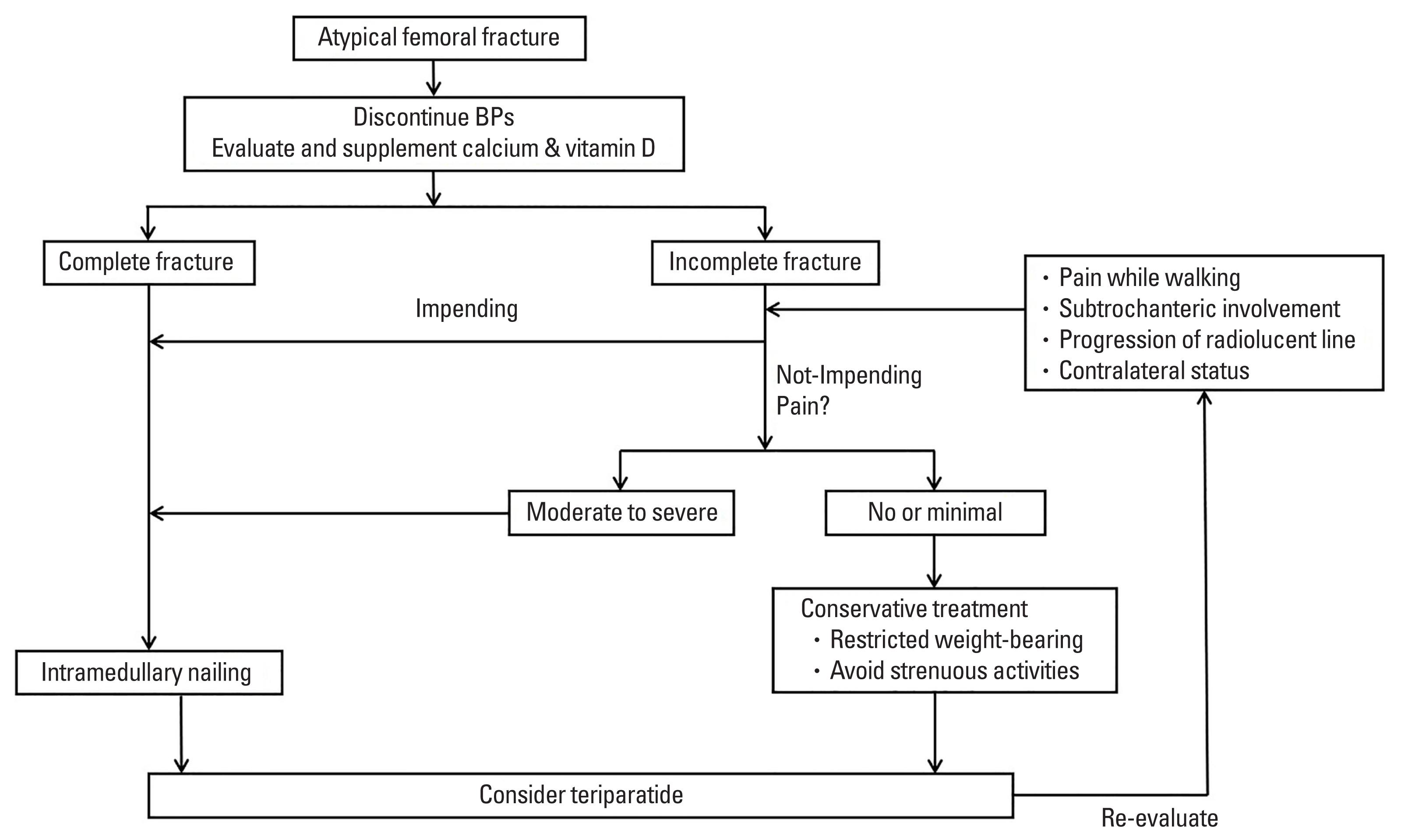
As the aging population increases, the number of patients with osteoporosis is gradually rising. Osteoporosis is a metabolic bone disease characterized by low bone mass and the microarchitectural deterioration of bone tissue, resulting in reduced bone strength and an increased risk of low-energy or fragility fractures. Thus, the use of anti-resorptive agents, such as bisphosphonates (BPs), to prevent osteoporotic fractures is growing annually. BPs are effective in reducing hip and other fractures. However, the longer a patient takes BPs, the higher the risk of an atypical femoral fracture (AFF). The exact mechanism by which long-term BP use affects the development of AFFs has not yet been clarified. However, several theories have been suggested to explain the pathogenesis of AFFs, such as suppressed bone remodeling, impaired bone healing, altered bone quality, and femoral morphology. The management of AFFs requires both medical and surgical approaches. BPs therapy should be discontinued immediately, and calcium and vitamin D levels should be evaluated and supplemented if insufficient. Teriparatide can be used for AFFs. Intramedullary nailing is the primary treatment for complete AFFs, and prophylactic femoral nailing is recommended if signs of an impending fracture are detected.
INTRODUCTION
Bisphosphonates (BPs) have been widely used as the primary treatment agents for osteoporosis in men and women since the early 1990s. Randomized controlled trials have demonstrated that BPs can reduce osteoporotic fractures by 40% to 70% in individuals with osteoporosis.[1] BPs act by inhibiting osteoclast function and inducing osteoclast apoptosis.[2] However, there are concerns about potential side effects associated with the excessive suppression of bone turnover. In 2005, reports emerged regarding unusual fragility fractures in the subtrochanteric and femoral shaft regions of patients undergoing long-term BP treatment. These fractures were subsequently defined as atypical femoral fractures (AFFs).
The exact pathogenesis of AFFs has not been fully elucidated, but it is believed that the severe suppression of bone turnover in AFF patients impairs healing at the fracture site, posing challenges for treatment.[3] AFFs primarily affect elderly patients with osteoporosis, leading to increased medical costs and decreased quality of life, thereby imposing socioeconomic burdens.[4,5]
The American Society for Bone and Mineral Research (ASBMR) published a task force report on AFFs in 2010,[6] followed by a revised case definition in 2013.[7] A position statement on AFFs was released in Korea in 2015.[8] As a decade has passed since the publication of the revised case definition, which currently serves as a guideline for AFF treatment, it is crucial to organize the existing evidence on AFFs based on updated research findings.
DEFINITION OF AFF
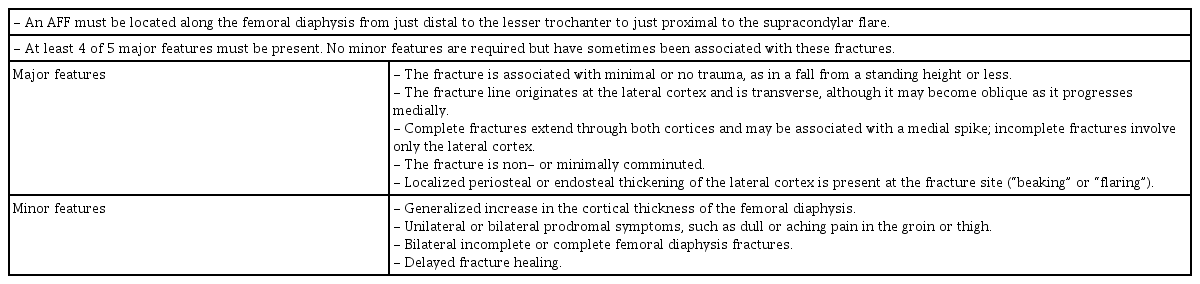
AFFs exhibit distinct characteristics that differentiate them from more common hip and femur fractures. The initial definition of an AFF was established by the ASBMR in their task force report of 2010. While these criteria proved helpful in defining AFFs, some fractures remained controversial. The ASBMR revised its AFF criteria in 2013, incorporating more information on epidemiology and morphology. The revised definition, presented in Table 1, requires the presence of at least 4 out of 5 major features to meet the criteria for AFF.[6,7] These major features highlight the atypical nature of the fractures, distinguishing them from other femur fractures associated with osteoporosis. The minor features describe conditions often related to AFFs, but they are not essential for diagnosis.
Although the ASBMR criteria provide clear guidelines, in practice, there may be some ambiguities in the definition, particularly when it comes to individual features or other aspects, such as the specific location of the fracture.[9]
EPIDEMIOLOGY
Between 2008 and 2016, the number of osteoporotic fractures (including hip, vertebral, humeral, and distal radius fractures) gradually increased in Koreans over the age of 50, regardless of gender. Thus, the use of anti-osteoporosis medications, such as BPs, to prevent osteoporosis and osteoporotic fractures is also increasing in Korea, with a yearly increase of 6% from 2011 to 2016.[10] While AFFs can occur in patients who have not been exposed to BP treatment, they most commonly occur in patients who have been taking BPs for several years.
Accurately evaluating the occurrence of AFFs is challenging due to the low incidence. The reported incidence varies greatly depending on the study design and subjects, ranging from 2.3 to 130 cases per 100,000 patient years.[6,7,11] The incidence of AFFs increases with the use of BPs and the duration of anti-resorptive treatment. Dell et al. [12] reported the incidence of AFF in the US and its relationship with BP use, indicating an incidence of 1.8, 38.9, and 107.5 cases per 100,000 patient-years associated with 2, 6 to 8, and greater than 10 years of BP use, respectively. Mahjoub et al. [13] demonstrated a statistically significant relationship between the occurrence of AFF and BP use (odds ratio, 10.39; 95% confidence interval, 2.22–48.58; P=0.0029).
Several studies have highlighted the higher association of AFFs with Hispanics and Asians, especially Koreans. One study reported an 8-fold higher incidence of AFFs in Asians compared to white women, suggesting differences in proximal femoral geometry as a possible reason.[14] Although the incidence of AFF is relatively higher in Asians than in other races, the proportion of AFFs among femur fractures is not high. Lee et al. [15] analyzed data from 16 tertiary medical institutions in Korea and reported that only 1.2% of 1,361 patients with proximal femoral fractures had AFFs.
PATHOGENESIS
AFF is considered to be the result of an imbalance between bone resorption and bone formation, leading to disrupted bone remodeling. The pathogenesis of an AFF involves multiple factors that contribute to its development. Gaining a comprehensive understanding of the underlying mechanisms is essential for the development of effective treatment strategies and preventive measures against these fractures.
1. BPs
BPs work by inhibiting osteoclastic activity, thereby preventing bone resorption. The maximum suppression of bone turnover was observed to occur approximately 3 months after starting BP administration.[16,17] The BP benefits in fracture reduction from short-term therapy for 3 to 5 years far outweigh the risks of AFFs.[18] However, long-term studies have consistently shown an increased incidence of AFFs with prolonged BP use. One study reported a 6-fold increase in the occurrence of atypical hip fractures after 5 to 8 years of BP use and a 13.1-fold increase after more than 8 years.[19] The precise mechanism by which long-term BP use affects the development of AFFs has not yet been fully elucidated. However, several hypotheses have been proposed based on various studies.[3,7,20–22]
1) Suppressed bone remodeling
BPs inhibit osteoclastic activity, resulting in decreased bone turnover. The prolonged suppression of bone remodeling can lead to the accumulation of microdamage in the bone, making it more susceptible to fractures.
2) Impaired bone healing
BPs have been demonstrated to have an impact on fracture healing by impeding the recruitment and function of osteoblasts, which play a crucial role in bone formation. This inhibition of osteoblast activity by BPs can lead to the impaired healing of stress fractures, potentially contributing to the development of AFFs.
3) Altered bone quality
Long-term BP use may affect the composition and quality of bone. Changes in mineralization, collagen cross-linking, and alterations in bone microarchitecture can compromise the mechanical properties of bone, increasing the risk of fractures.
These bone changes lead to a deviation from normal osseous composition, which promotes resistance to plastic deformation and reduces elastic behaviors, making the bone vulnerable to fractures.[23] More recently, AFFs have been observed in randomized control studies of the biological anti-resorptive agent denosumab.[24–26]
2. Fracture location and femoral morphology
Several studies have indicated that certain geometrical features of the femur can influence the strain experienced by the femoral diaphysis. Increased lateral and anterior bowing of the femur has been strongly associated with higher mechanical strain on the femur, specifically at sites prone to AFFs.[27] Compared to controls, patients with AFFs had excessive femoral offset (43.1 mm vs. 38.3 mm; P=0.0007), proximal femoral neck angle in varus (128.9 degrees vs. 134.0 degrees; P<0.0001), and greater proximal cortical thickness. This retrospective study not only confirmed the significant association between AFF occurrence and BP exposure but also highlighted the potential contribution of proximal femoral geometry to the development of an AFF.[13]
DIAGNOSIS
The increasing incidence of AFF warrants a high index of suspicion and further examinations of patients who have been taking BPs for more than 5 years and present with dull pain and tenderness in the thigh.[28] Plain radiographs often reveal characteristic findings, such as beaks or flares in the lateral femoral cortex, including the periosteal and/or intraosseous callus. In some cases, "dread black lines" may also be observed in the lateral cortex.[29,30] If the plain radiograph appears normal despite prodromal symptoms, additional imaging modalities, such as bone scans or magnetic resonance imaging (MRI), can be utilized to identify hidden lesions in the femur.
The differential diagnosis between AFF and other pathologic fractures, such as stress fracture, hypophosphatasia, and osteogenesis imperfecta, is important. It is important to note that stress fractures or hypophosphatasia typically originate from the medial aspect of the femur rather than the lateral cortex.[28]
A recent study explored the potential of extended femoral dual energy X-ray absorptiometry (DXA) scans. Such scans could be valuable in detecting early or focal cortical thickening in the lateral femur. However, further research is needed to determine DXA scan features that warrant radiologic follow-up. Nevertheless, this technique shows promise as it could potentially help identify patients at risk of complete AFF, particularly through prodromal pain assessment.[31]
MEDICAL TREATMENT
The ASBMR has recommended the temporary discontinuation of BPs.[32] Once a patient is diagnosed with AFF, BP treatment must be discontinued, even in cases of incomplete fractures, to prevent progression to a complete fracture.[6,7] Calcium and vitamin D levels should also be evaluated and supplemented if insufficient.[33] Patients with incomplete fractures need to avoid strenuous activities, and if necessary, weight-bearing can be restricted. If the pain persists throughout more than 3 months of medical treatment, prophylactic surgical nail fixation is recommended to prevent a complete fracture.[7,28]
Teriparatide, a recombinant form of parathyroid hormone, can be used for AFF based on its ability to improve fracture healing. Teriparatide, either alone or as an adjunct to surgical fixation, has shown potential in promoting the healing of AFFs.[34,35] Several studies reported that teriparatide promoted bone union in osteoporotic fractures.[36–38] Although randomized controlled trials specifically focusing on AFF have not been conducted, teriparatide is considered a viable treatment option for an AFF adjunct to standard treatment.[39–41] There is no consensus on treatment strategies after teriparatide treatment in AFF patients. There are only recommendations for clinical practice based on experiments through some studies.[42]
SURGICAL TREATMENT
AFFs are found as incomplete and complete fractures, and surgical treatment is inevitable in the case of complete fractures.[43] Intramedullary nailing is the first-line treatment for complete AFFs because fixation using a metal plate is more invasive, as it requires fixing the entire length of the femur. Additionally, bone remodeling by osteoclast is often suppressed in patients with AFFs, so delayed direct bone healing is highly likely.[3,44] Intramedullary fixation promotes secondary bone healing through endochondral ossification, which is less affected by osteoclast function suppression. Furthermore, compared to a metal plate, the intramedullary nail has a mechanical advantage as it is positioned more medially.[45] AFFs exhibit a higher incidence of nonunion compared to other types of fractures. In some cases, closed reduction is challenging for AFFs, but closed reduction should be attempted first to avoid the high risk of delayed union or nonunion due to blood flow damage to the fracture site associated with open reduction.[46,47] The risk of nonunion increases if there is incomplete contact with the lateral cortical bone. Therefore, careful attention should be paid to entry point selection when inserting the intramedullary nail to prevent varus deformation at the fracture site.[48–50]
Over-reaming is recommended due to intramedullary sclerosis at the fracture site.[46] Care should be taken when inserting an intramedullary nail, as iatrogenic fractures can easily occur when the nail passes the fracture site due to sclerotic changes. The risk of delay and nonunion is high when iatrogenic fractures occur.[47,51]
Most patients with AFFs have an anterolateral bowing of the femur. Thus, the intramedullary nail may not fit the shape of the femur.[52] Various methods have been reported to overcome bowing during intramedullary nailing in patients with severe femoral bowing. Firstly, the entry point of the intramedullary nail is moved from the piriformis fossa to the lateral position (greater trochanter), and a relatively small diameter nail can be used. Kim et al. [53] reported positive outcomes using a lateral entry point in AFF patients with severe anterolateral bowing. Although there was no difference in the degree of union, the time to union with the lateral entry point decreased significantly. Secondly, a method using the opposite side of the intramedullary nail (A2FN; Synthes, Solothurn, Switzerland) can be employed to reduce the risk of mismatch between the nail and femoral bowing. However, special caution is required when considering this method.[52] Thirdly, ipsilateral nails with an anterior curvature can be inserted with external rotation, allowing the external rotation of the nail with anterior bowing to match the shape of the laterally bowed femur.[54] However, inserting the interlocking screw can be challenging with this method. Finally, in cases where intramedullary nail insertion is difficult with the aforementioned methods, fixation can be performed using a plate. In such cases, minimally invasive plate osteosynthesis principles should be followed, and the plate should cover the full length of the femur to ensure sufficient working length.[50]
Of the patients with AFF, 28% to 44.2% have bilateral involvement.[55,56] Therefore, once diagnosed with an AFF, careful examination of both sides is required. Plain radiographs of the contralateral femur should be taken to check for fractures. If a fracture is suspected, technetium bone scintigraphy or MRI can be additionally performed (Fig. 1).
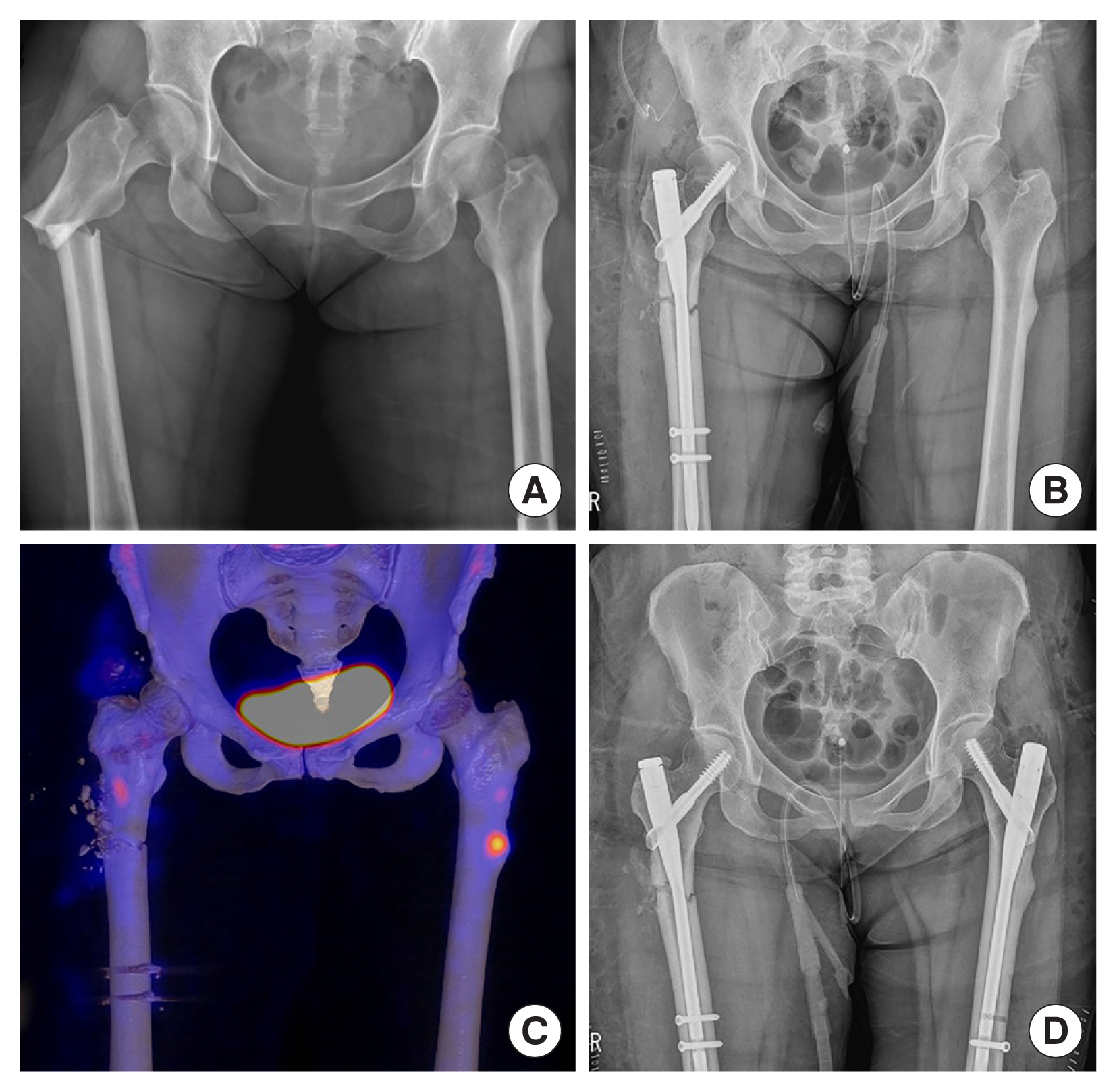
Radiographs of a 51-year-old postmenopausal woman with an atypical femoral fracture. (A) Plain anterior-posterior radiograph of the right femur reveals a subtrochanteric transverse fracture line that becomes oblique as it progresses medially. The left femur shows periosteal thickening in the subtrochanteric area, resulting from chronic stress on the lateral femoral cortex. (B) Postoperative plain radiograph showing the use of a cephalomedullary nail for a complete fracture on the right side. (C) Bone single-photon emission computed tomography images taken after internal fixation of the right femur with a cephalomedullary nail exhibit focal increased radio-uptake with cortical thickening in the lateral aspect of the left proximal femur. (D) Postoperative plain radiograph showing additional prophylactic fixation of an incomplete left fracture.
When an incomplete fracture is found, it is important to differentiate whether it is an impending fracture with a high possibility of progressing to a complete fracture. Prophylactic fixation should be performed for impending fractures. It is known to be an impending fracture in case of subtrochanteric involvement, worsening pain during walking, and a radiolucent line (Fig. 2).[39,57]
CONCLUSION
AFFs occur predominantly in patients who have been using BPs for the prevention of osteoporotic fractures. Although the incidence of AFFs is not high, AFF characteristics differ from those of normal fractures, such as difficulty in performing fracture surgery and a high risk of delayed union or nonunion. Therefore, it is necessary to understand the characteristics of these AFFs to treat them appropriately.
Notes
Ethics approval and consent to participate
Not applicable.
Conflict of interest
Young-Kyun Lee has been the Editor-in-chief of the Journal of Bone Metabolism since January 1, 2022, but has no role in the decision to publish this article. Except for that, no potential conflict of interest relevant to this article was reported.